
Lung Cancer Treatment in Singapore
Lung cancer is one of the biggest health challenges in Singapore, but with advances in detection and lung cancer treatment, especially minimally invasive thoracic surgery, there is hope.
At Neumark Lung & Chest Surgery Centre, led by Dr Harish Mithiran, we provide comprehensive, patient-centric lung cancer care that integrates cutting-edge diagnostics, molecular-guided therapy, and precision surgery to deliver top-tier care. Ensuring patients receive expert and tailored care, our multidisciplinary team at Gleneagles and Mount Alvernia hospitals comprises experienced cancer specialists.
Whether you have an early-stage lung cancer tumour or complex metastatic disease, every decision is informed, timely and personal for you.
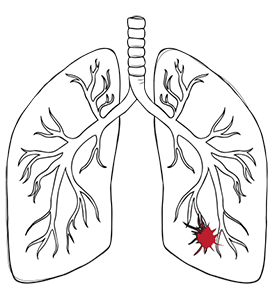
What Causes Lung Cancer?
Genetic mutations in the DNA of airway cells cause lung cancer. While cigarette smoking is a significant risk factor, other risk factors include exposure to asbestos, family history of lung cancer, and certain genetic predispositions. What causes lung cancer?
Exposure to other environmental toxins, such as radon, can also cause these mutations and increase the risk of developing lung cancer. In cases of lung cancer, the damaged, abnormal cells can multiply uncontrollably and destroy normal cells. Some individuals develop lung cancer, which can spread throughout the entire lung and metastasise to different parts of the body.
In recent years, there has been an increase in lung cancer cases in Singapore among never smokers. Lung diseases such as chronic obstructive pulmonary disease (COPD) can also increase the risk of developing lung cancer.
Types of Lung Cancer
There are two main types of lung cancer, each with distinct characteristics and prevalence rates.
An aggressive, fast-growing type of lung cancer in which the cells are small and oval under a microscope. Small-cell lung cancer is most strongly linked to smoking and tends to spread (metastasise) to other parts of the body. In small-cell lung cancer, two stages are identified: the limited and extensive stages, based on the extent of cancer spread.
The most common type of lung cancer accounts for about 85% of all lung cancer. Non-small cell lung cancer is defined as any epithelial lung cancer other than small cell lung cancer, characterised by larger cells that grow more slowly than small cell lung cancer. Non-small cell lung cancer includes subtypes such as adenocarcinoma, squamous cell carcinoma, and large cell carcinoma.
Cancer cells in the lungs can interfere with normal cells, affecting lung function and breathing. Identifying cancer cells in biopsy specimens is crucial for confirming a lung cancer diagnosis and planning lung cancer treatment.

Lung Cancer in Singapore
Lung cancer in Singapore is the second most common cancer in men and the third most common cancer in women. According to the Singapore Cancer Registry (2018-2022), 9,012 lung cancer cases were diagnosed over 5 years, accounting for 13.7% of all male cancers and 7.7% of female cancers. It is also the leading cause of cancer death in men and the second in women.
A local trend is the increasing incidence among never smokers, especially Singaporean women. Nearly 48% of non-small cell lung cancer cases occur in individuals with no smoking history. This is driven mainly by EGFR gene mutations (which may cause lung cancer cells to grow), which are found in up to 60% of never-smoking Asian patients. Environmental factors such as urban air pollution, like haze episodes and second-hand smoke, further compound the increased risk.
At Neumark, we understand these patterns. Our lung cancer screening Singapore and treatment strategies go beyond traditional risk profiles to include younger patients, non-smokers, and those with a family history or genetic predisposition to lung cancer.
Lung Cancer Symptoms
Common signs of lung cancer, such as coughs, chest pains and shortness of breath, can often be mistaken for other conditions. In the early stages of lung cancer, lung cancer symptoms are frequently absent, making early detection and diagnosis particularly challenging. Many patients may not notice any early signs of lung cancer until the disease has progressed.
In more advanced stages, lung cancer may present with additional common symptoms such as:
Pleural effusion (fluid buildup around the lungs)
Severe fatigue
Bone pain if the cancer has spread to the bones

Neurological symptoms if there’s brain involvement
Unexplained weight loss
Hoarseness or difficulty swallowing
Please note that the presence of these symptoms doesn’t mean lung cancer, but they do warrant medical attention. Early detection can impact lung cancer treatment options and outcomes. If you have persistent respiratory symptoms or unexplained changes in your health, it’s best to consult a lung cancer specialist in Singapore, like Neumar,k for a thorough evaluation to see if you have early symptoms of lung cancer.
Lung Cancer Diagnosis
Neumark’s private lung cancer treatment centre offers same-day consultations for all patients, whether private or referred by other doctors. After your initial consultation, diagnostic tests and imaging tests, such as imaging scans and biopsies, are essential procedures used to confirm a lung cancer diagnosis and diagnose lung cancer accurately.
Our staging workup is rapid and systematic to ensure lung cancer is accurately diagnosed and staged, with lung cancer diagnosed through comprehensive testing. This streamlined process is done in one week at Gleneagles or Mount Alvernia hospitals, so there is no delay between diagnosis and treatment planning. A medical oncologist may review diagnostic results and recommend further treatment for lung cancer.
High-Resolution CT Scans
Of the chest-abdomen-pelvis with contrast to assess the tumour size and nodal disease
PET-CT Scans
Positron emission tomography to detect metabolic activity in lymph nodes and distant sites
Brain MRIs
Magnetic resonance imaging for all patients with Stage III suspicion or neurological symptoms
Endobronchial Ultrasounds (EBUS)
For minimally invasive mediastinal node sampling (95% sensitivity)
Multidisciplinary Tumour Board (MDT)
Reviews within 48 hours of final imaging by a multidisciplinary team

How Lung Cancer Is Staged
Lung cancer stages are determined using the TNM (Tumour, Node, Metastasis) system. The stage of lung cancer indicates how far the cancer has spread to other parts of the body and guides treatment decisions.
- T describes the size and extent of the primary tumour (T1–T4)
- N indicates regional lymph node involvement (N0–N3)
- M denotes distant metastasis (M0 or M1)
Staging determines whether the cancer is localised (Stage I in early stages), regionally advanced (Stage II–III in advanced stages) or metastatic (Stage IV in more advanced stages). Accurate staging is the foundation of effective treatment, as the lung cancer depends on the stage, cancer type, and the patient’s overall health.
Related LUNG CANCER STAGES & TREATMENT

Lung Cancer Treatment by Stage
The approach to treatment for lung cancer depends on the stage of the disease, the patient’s overall health and other patient-specific factors. Below is a clear evidence-based pathway:
Stage | Primary Approach | Neumark’s Surgical Role |
I–II | Anatomic resection + systematic nodal dissection | VATS / RATS / U-VATS lobectomy or segmentectomy |
III | Neoadjuvant chemo/immunotherapy → surgery or definitive chemoradiation | Selective resection post-response via RATS for central or complex tumours |
IV | Systemic therapy first; local control for oligometastasis | VATS wedge resection for solitary brain, adrenal, or lung metastases after targeted therapy response |
Chemotherapy is used to treat lung cancer and works by targeting and killing rapidly dividing cancerous cells to destroy cancer cells. There is a 70% 5-year lung cancer survival rate when detected at Stages I & II in early stages.
Lung Cancer Surgery
Lung cancer surgery and lung cancer operation can be done minimally invasively. Neumark surgeons utilise three different types of minimally invasive surgeries for lung cancer:
Robotic-Assisted Thoracic Surgery (RATS) is used for some thoracic procedures, including lung cancers and mediastinal growths.
Video-assisted Thoracic Surgery (VATS) uses small incisions and a camera to remove cancerous tissue. Surgeons insert a thoracoscope with a camera through a small cut to see inside the chest and instruments through other small incisions to do the surgery.
Uniportal Video-Assisted Thoracic Surgery (U-VATS) assesses and treats lung and mediastinal diseases through a single incision.
For each type of surgery, preoperative assessments and risk management are crucial to achieving optimal outcomes and ensuring patient safety through surgical procedures.
Lung cancer surgery may involve removing a segment (segmentectomy), a lobe (lobectomy) or the entire lung (pneumonectomy), depending on the size and stage of the tumour. During these surgical procedures, the surgeon will also remove surrounding lymph nodes and nearby lymph nodes to ensure complete cancer removal and staging. Tissue samples from these lymph nodes will be sent to the lab to see if the cancer spread. After lung cancer surgery, patients may receive further chemotherapy to clear up any remaining cancer cells.
After your lung cancer is removed, we will schedule post-operative consultations to check on your functional health after lung cancer resection.
Schedule a Consultation
Pre-Op & Post-Op

Pre-op preparation involves a comprehensive evaluation to ensure the best outcome. This includes a physical examination, lung function test, blood tests and imaging tests to assess your overall health and fitness for surgery. If you smoke, quitting at least 2 weeks before surgery can reduce complications and support recovery.
Your treatment plan will be developed by a multidisciplinary team that includes thoracic surgeons from thoracic oncology, medical oncologists from medical oncology, and radiation oncologists from clinical oncology to ensure all aspects of your care are considered. After lung cancer surgery, you may have a chest tube to prevent fluid or air accumulation, along with pain management strategies to keep you comfortable. Early mobilisation and walking are encouraged to help your lungs expand and speed up recovery.
Regular follow-up and scans are essential to monitor progress, detect cancer recurrence and address any questions or concerns you may have as you recover.
Oligometastatic NSCLC

Up to 20 percent of Stage IV patients present with oligometastatic disease, that is, a cancer condition with fewer than 5 metastases. After 3-6 months of targeted therapy (e.g. osimertinib for EGFR) or immunotherapy treatment, patients who achieve a primary response may benefit from local consolidative treatment.
At Neumark, we perform VATS wedge resection for peripheral lung tumours or RATS for hilar control, reducing blood flow through blood vessels to the lung. Studies show this approach extends progression-free survival from 6 to 14 months. All cases are reviewed by our weekly multidisciplinary team, which includes thoracic surgeons, medical oncologists, radiation oncologists and interventional radiologists.
Related Lung Cancer Conditions
Molecular Testing for Targeted Therapy
Molecular profiling is mandatory for every new diagnosis of adenocarcinoma or non-squamous non-small cell lung cancer. At Neumark, we use next-generation sequencing (NGS) to test for actionable alterations and genetic mutations:

Mutation | Prevalence in Singapore Never-Smokers | First-Line Therapy |
EGFR (exon 19/21) | 50–60% | Osimertinib |
ALK rearrangement | 5–7% | Alectinib |
ROS1 fusion | 2% | Entrectinib |
BRAF V600E | 1–2% | Dabrafenib + Trametinib |
MET exon 14 skipping | 3% | Capmatinib |
RET fusion | 1–2% | Selpercatinib |
NTRK fusion | <1% | Larotrectinib |
PD-L1 expression ≥50% | 30% | Pembrolizumab monotherapy |
Results are available in 7-10 days via needle biopsy or liquid biopsy (ctDNA – circulating tumour DNA) using radioactive material. This enables same-cycle treatment initiation, improving survival in mutation-positive patients.
Non-Surgical Options: Immunotherapy & SBRT
While surgery is our core strength, we work seamlessly with non-surgical therapies:

Immunotherapy for lung cancer is an option for patients who are not suitable for surgery, chemotherapy or radiotherapy or when these have been exhausted. Immunotherapy works by activating the body’s immune system to kill cancer cells and treat cancer. Drugs like immune checkpoint inhibitors help the immune system recognise and attack cancerous cells by blocking proteins that prevent immune cells from attacking them. Immunotherapy can be used alone, with chemotherapy or after chemoradiotherapy, depending on the cancer type and stage.
Stereotactic Body Radiotherapy (SBRT), a form of radiation therapy, is a non-invasive radiation treatment that uses multiple high-dose beams to target and destroy lung tumours in a few outpatient sessions. This form of stereotactic body radiotherapy is designed to kill cancer cells in targeted areas. It is a standard cancer treatment for early-stage lung cancer, medically inoperable lung cancer and also for early-stage operable disease, recurrent disease or lung metastases. Radiation therapy can also be used as palliative treatment to relieve symptoms in advanced cases of lung cancer.
Lung Cancer Screening in Singapore
Early detection saves lives. The Health Promotion Board (HPB) and World Health Organization recommend annual low-dose CT (LDCT) screening for those:
- Ages 55–74
- ≥20 pack-year smoking history
- Quit smoking <15 years ago
Never-smokers with a strong family history or known EGFR risk may also qualify via specialist referral.

Neumark offers a comprehensive lung cancer screening package in Singapore:
Test | Specifics |
Low-Dose Computed Tomography (LDCT) Imaging Test | Specialised 3D technology produces detailed images of the lung Superior imaging capabilities compared to X-rays Detects lung abnormalities, including nodules and lung tumours Quick and painless |
Cardiopulmonary Exercise Testing | Monitors heart rate, blood pressure, oxygen consumption and carbon dioxide production Indicates a lung function abnormality if exercise capacity is impacted Assesses lung function |
Pulmonary Functional Test | Measures lung volume, capacity, rates of flow and gas exchange Detects narrowing of the lungs’ airway. |
Review and Analysis | Dr Harish Mithiran expertly analyses results Diagnosis is promptly provided if abnormalities are detected Personalised treatment plan Minimally invasive treatments are proposed to reclaim health. |
Schedule a Consultation

Neumark Lung Cancer Treatment Centre in Singapore
Concerned about a persistent cough, chest discomfort or an abnormal scan? At Neumark Lung Cancer Treatment Centre, you won’t have to wait in the dark. Led by senior consultant thoracic surgeon Dr Harish Mithiran, a premier lung cancer specialist in Singapore with clinical interests in lung cancer care, our team gets you from concern to clarity with same-day or next-day imaging, specialist review and a clear plan you can trust.
Your care is coordinated across Gleneagles Hospital on Napier Road and Mount Alvernia Hospital on Thomson Road, with access to advanced diagnostics, bronchoscopy and image-guided biopsy. When treatment is needed, we tailor it to your cancer biology and stage, offering minimally invasive lung cancer surgery, such as VATS, U-VATS, or robotic techniques where appropriate, alongside oncology partners for targeted therapy, immunotherapy, and precision radiotherapy.
If you suspect lung cancer or have been told you have a lung nodule, don’t wait. Book a prompt consultation with Neumark today and get a definitive answer and a plan that puts you back in control. Early action changes everything. Let us guide you to the best possible outcome.
FAQs about Lung Cancer Treatments
Staging includes TNM classification, PET-CT, brain MRI, and EBUS nodal sampling, all completed within 1 week.
All patients with NSCLC; results guide targeted therapy and are ready in 7–10 days.
There is no single answer to this, as lung cancer cases vary, though treatment outcomes are usually better when detected early.
Most patients go home in 2–3 days and back to desk work in 1–2 weeks.
For inoperable early-stage tumours or oligometastatic control after systemic therapy.
EGFR mutations, second-hand smoke, air pollution and genetic predisposition.
In PD-L1 ≥50% cases, 40% achieve a durable response.
CT scans every 6 months for 2 years, then annually.
Most Integrated Shield Plans cover LDCT for high-risk individuals.
DISCLAIMER: The information provided on this website is for general informational purposes only and is not intended as a substitute for professional medical advice, diagnosis, or treatment. The use of this website does not create a doctor-patient relationship and no medical advice should be inferred or assumed. It is the user’s sole responsibility to seek the advice of their healthcare professionals for any medical concerns they may have and the user should not disregard, or delay, prompt medical advice for any such condition.
