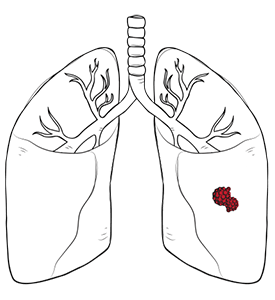

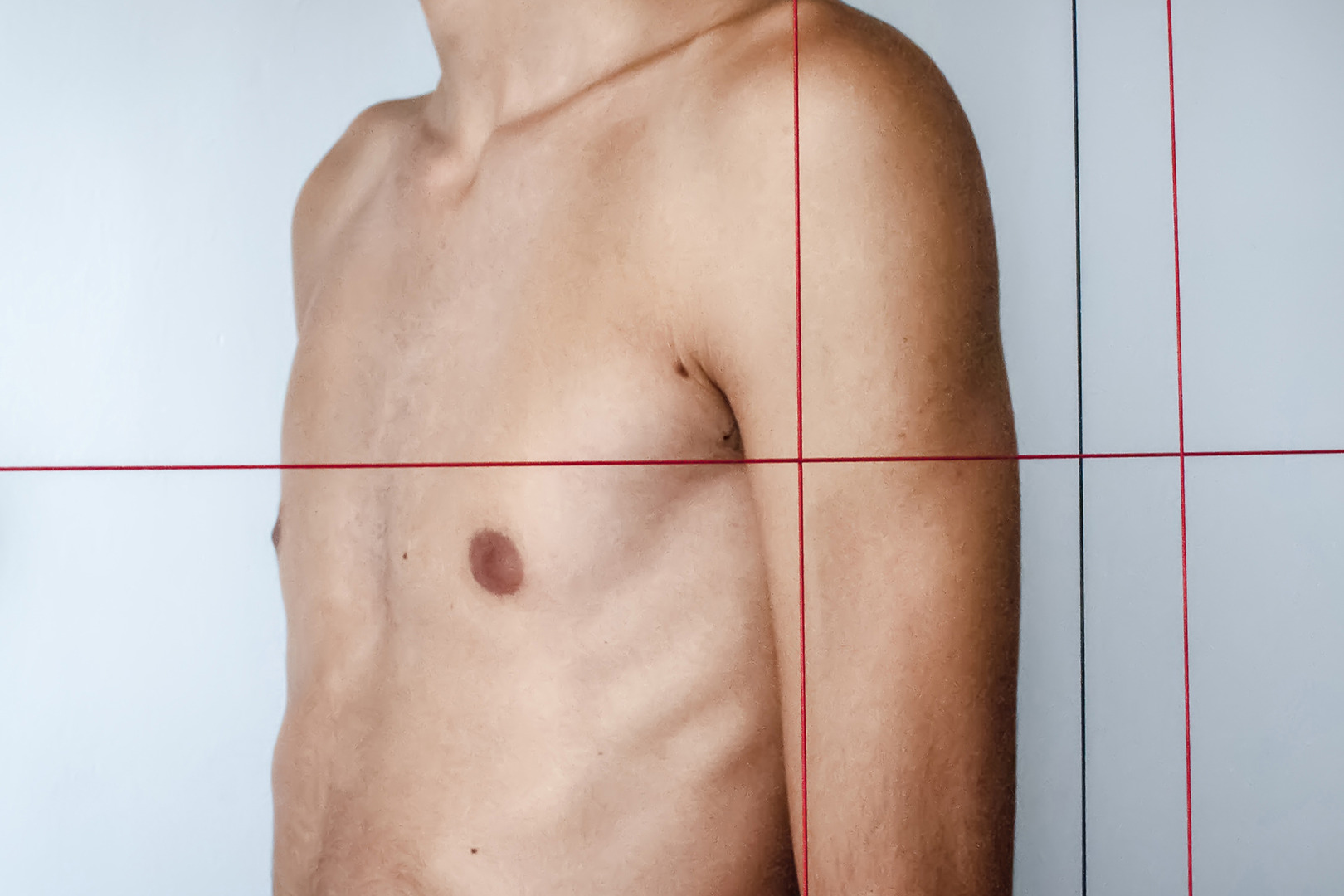
Pectus excavatum, also known as ‘funnel chest’, is one of the most common congenital chest wall deformities, affecting about 1 in 400 births. An inward depression of the sternum and costal cartilages characterises this condition. It often results in a deep dent or sunken breastbone in the middle of the chest, especially in severe cases where the breastbone is recessed.
The cause of pectus excavatum is not fully understood, but it does run in families. Knowing what pectus excavatum is and what it means is crucial for patients and families dealing with this condition.
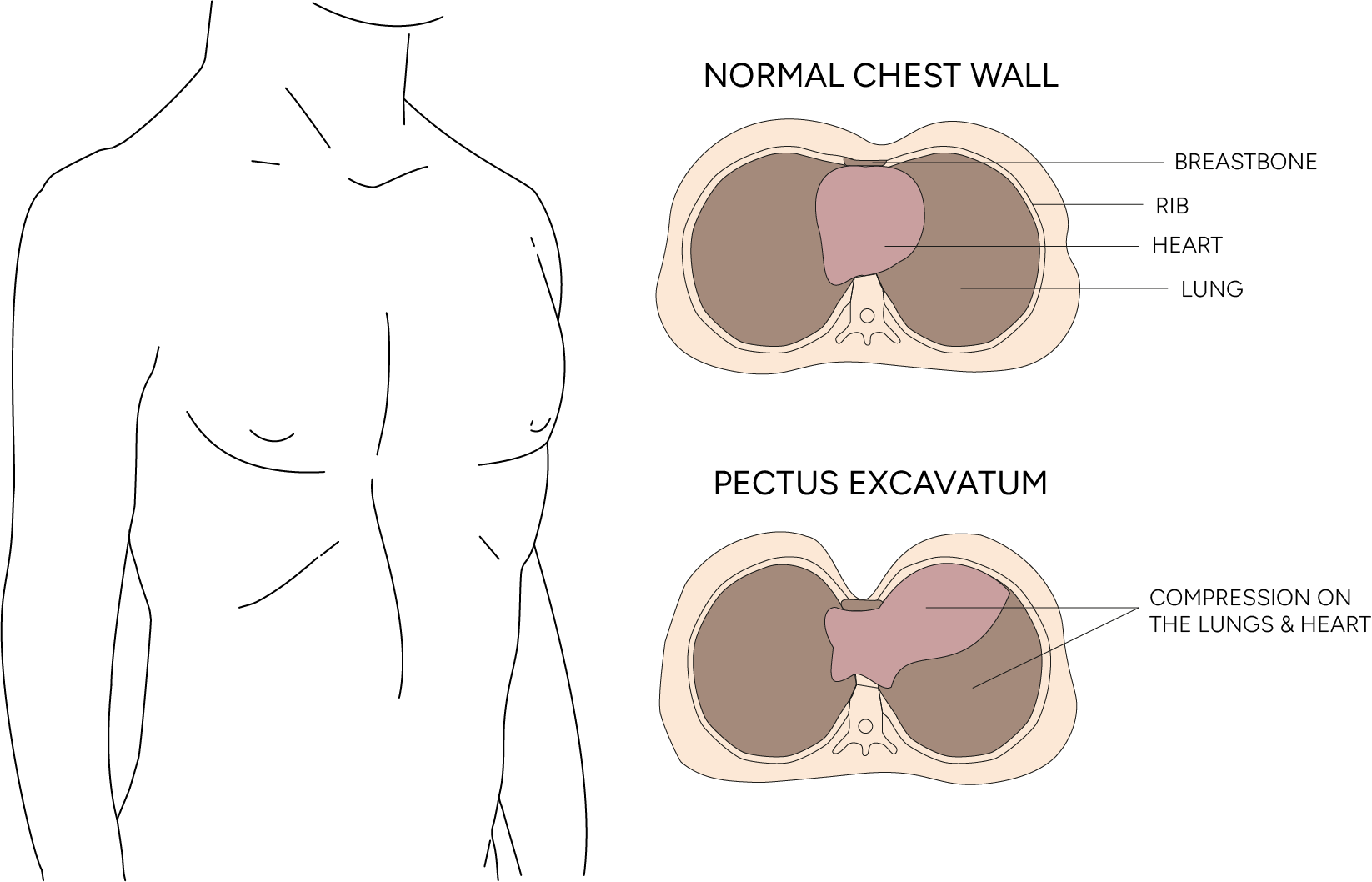
Some people have minimal symptoms while others have significant respiratory and cardiac problems. The ‘caved in’ chest appearance of pectus excavatum is due to abnormal growth of the cartilage that connects the ribs to the breastbone, causing the sternum to curve inwards.
The rib cage is also affected and contributes to the sunken appearance, and potentially the structure of the anterior thoracic wall. The compressed chest cavity can limit lung expansion, reduce vital capacity and cause shortness of breath with exercise. The heart can also be displaced and compressed, reducing cardiac output and exercise tolerance.
Beyond the physical issues, the psychological impact cannot be ignored. Many patients, especially adolescents and young adults, have profound body dysmorphic disorder about their appearance. Psychological symptoms like anxiety or low self-esteem are common, and this emotional burden often leads to social withdrawal, avoidance of activities that require chest exposure and decreased quality of life.
The most obvious sign is a sunken or concave chest, which may be present from birth, or become more pronounced during periods of rapid growth, like puberty. In mild pectus excavatum, the indentation may be subtle and cause no discomfort, while in severe cases it can cause pectus excavatum complications, such as chest pain, shortness of breath and even heart or lung problems.
Diagnosis starts with a thorough physical examination by a thoracic surgery specialist who will assess the depth and symmetry of the chest wall deformity. Imaging studies, like a chest X-ray or CT scans, are necessary to evaluate the extent of the condition and its effect on the heart and lungs. These diagnostic tools will also determine if surgery is needed, or if non-surgical options like vacuum bell therapy may be appropriate. Early and accurate diagnosis ensures patients get the best care tailored to their needs.

The causes of pectus excavatum are not fully understood, but research suggests both genetic and developmental factors are involved. One of the principal risk factors is a strong hereditary component, with about 25% of cases showing familial clustering. This genetic predisposition means certain individuals inherit a tendency to abnormal cartilage growth patterns that manifest during periods of rapid skeletal development. Other risk factors are genetic and familial influence, which increase the likelihood of developing the condition.
Current theories suggest that an imbalance in the growth rates of the sternum and costal cartilages during foetal development and early childhood creates the deformity. Some researchers propose that the pectus excavatum effects, such as abnormal diaphragmatic attachments, contribute to the condition, while others focus on intrinsic cartilage abnormalities.
Environmental factors may also play a role in the development or severity of the condition. Certain connective tissue disorders, like Marfan syndrome and Ehlers-Danlos syndrome, are associated with an increased incidence of pectus excavatum. Though some studies suggest respiratory infections during early childhood may exacerbate the condition, this is still a topic of debate in the medical community.

The choice of how to fix pectus excavatum depends on multiple factors, including the severity of the deformity, age of the patient, presence of symptoms and individual preferences. The treatments range from conservative management to advanced surgical interventions.
Conservative management usually involves physical therapy, breathing exercises and postural training. These can be helpful for mild cases or as an adjunct to surgery. Specialised exercise programmes focusing on chest expansion and core strengthening can improve respiratory function and posture, but rarely correct the underlying structural abnormality. Older children and adolescents may require different approaches or additional supervision during treatment, as their needs and responses can be different from those of younger patients.
Pectus excavatum can be treated with both surgical and non-surgical methods, depending on the case. For patients with significant symptoms or psychological distress, surgery often provides the best pectus excavatum treatment. The evolution of surgical techniques has improved outcomes and reduced complications, making surgery an option for many patients who previously had limited treatment choices.
The pectus excavatum Nuss procedure is a minimally invasive surgical treatment, an alternative to open reconstruction. Developed by Dr. Donald Nuss in the 1980s, this has become the gold standard for pectus excavatum surgery worldwide and has changed the treatment landscape for patients with pectus excavatum.
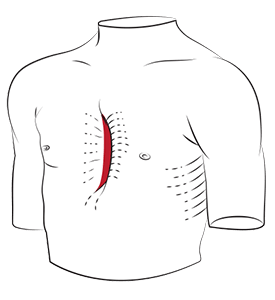
The pectus excavatum Nuss procedure involves placing a curved metal bar under the sternum through small incisions on each side of the chest. Called a ‘pectus bar’, this pushes the sternum and costal cartilages outwards with the primary goal of moving the sternum outwards to restore normal chest anatomy. The procedure addresses the lower breastbone, which is often the most deformed part in pectus excavatum cases. The bar remodels the chest wall over time. The procedure takes about 1-2 hours and is performed under general anaesthesia with thoracoscopic guidance for added safety and precision.
One of the most significant advantages of the pectus excavatum Nuss procedure is its minimally invasive nature. Unlike open techniques that require large incisions and cartilage removal, the Nuss procedure preserves the natural chest wall architecture and achieves excellent cosmetic and functional results. This means reduced postoperative pain, shorter hospital stays and faster recovery times compared to traditional surgical methods.

The ZipFix system provides added security and simplified bar removal. This system uses a unique attachment mechanism that offers optimal bar stabilisation and reduces the complexity of the removal procedure. Combining ZipFix with the Nuss procedure has shown promising results in lowering bar displacement and long-term stability. This addresses one of the main concerns with pectus excavatum surgery: bar migration or rotation, which can compromise surgical outcomes and require further interventions. Proven surgical techniques with innovative fixation systems give the best possible outcomes for patients seeking definitive treatment for their condition.
The Ravitch surgical procedure is a tried and tested approach for pectus excavatum surgery, especially for patients with severe symptoms or complex chest wall deformities. Unlike the minimally invasive technique, the Ravitch procedure is an open surgical approach allowing the surgeon direct access to the chest wall. During the operation, deformed cartilage is removed, and the breastbone is repositioned to a more normal position, restoring the natural shape of the chest.
This procedure is beneficial for patients who have not responded to non-surgical treatment or for those whose anatomy is not suitable for minimally invasive repair. The Ravitch technique can reduce chest pain, improve lung function and improve the appearance of the chest, leading to better physical and psychological outcomes. Although more invasive than newer methods, its long track record of success makes it a good option for pectus excavatum in select cases.
Proper preparation before pectus excavatum treatment is key to achieving the best possible results. Before surgical correction (either the Nuss or Ravitch procedure), patients will undergo a thorough evaluation, including lung function tests and physical examination. This helps the surgical team tailor the approach to each individual’s needs and ensure the patient is an ideal candidate for surgery.
Pain management is another crucial aspect of pre-treatment planning. Advances in pain control have improved the recovery experience, and discussing options with your surgeon can help set realistic expectations for the postoperative period. In some cases, optimal correction may require more than one bar or even multiple surgeries, especially in patients with complex or severe deformities.
In the Nuss procedure, the surgeon makes small incisions on each side of the chest to insert a curved metal bar under the breastbone. This bar is carefully positioned to lift the sternum into a more normal position and is secured in place with surgical hardware to ensure stability. Minimally invasive techniques, which use smaller incisions and special cameras to visualise the surgery, have become the standard for many patients with reduced scarring and faster recovery times. During the operation, the surgical team monitors the patient’s vital signs and takes every precaution to ensure safety and success.

While surgical intervention gives the most dramatic improvement for patients with pectus excavatum, comprehensive care goes beyond the operating theatre. Successful pectus excavatum treatment requires a multidisciplinary approach that addresses both physical and psychological aspects of the condition.
Postoperative care focuses on pain management, respiratory therapy and a gradual return to normal activities. The recovery process takes several weeks of limited activity followed by a gradual progression back to full function. Physical therapy plays a key role in optimising outcomes, helping patients regain strength and mobility while protecting the surgical repair.

The cost of pectus excavatum surgery is a concern for patients and families considering treatment options. While the upfront cost can be high, it’s important to consider the long-term benefits of surgical intervention, including an improved quality of life, physical function and psychological well-being.
Pectus excavatum surgery cost varies depending on several factors, including the complexity of the procedure, hospital stay and postoperative care. In Singapore, the cost structure is generally transparent, with patients receiving detailed estimates that outline all associated costs. Many insurance plans cover pectus excavatum surgery when medically necessary, though coverage varies depending on the policy and severity of the condition.
When evaluating pectus excavatum surgery cost, patients should consider the comprehensive nature of the treatment package. This includes preoperative evaluation, surgical procedure, hospital stay, postoperative care and follow-up appointments. The investment in experienced surgical teams and facilities contributes to better outcomes and reduced risk of complications, potentially reducing long-term healthcare costs.
The expertise of pectus excavatum surgeons is key to achieving optimal outcomes. This speciality requires extensive training in thoracic surgery, paediatric surgery and chest wall reconstruction. Surgeons with significant experience in pectus excavatum surgery understand the nuances of patient selection, surgical technique and postoperative management that contribute to successful outcomes.
When choosing a pectus excavatum surgeon, patients should consider factors such as surgical volume, training background and institutional support. High volume centres with dedicated chest wall programs offer the most comprehensive care with access to advanced imaging, specialised nursing care and multidisciplinary support teams.
The relationship between surgeon and patient is crucial in pectus excavatum surgery as the decision-making process involves weighing complex factors such as symptom severity, functional impairment and patient preferences. Experienced surgeons can guide patients through this decision-making process and provide realistic expectations and comprehensive information about treatment options.
Surgeons for pectus excavatum in Singapore, like Dr Harish Mithiran at Neumark Lung & Chest Surgery Centre, are trained in the latest surgical techniques and have access to minimally invasive technology. At Neumark, our team of experienced pectus excavatum surgeons is dedicated to providing world-class care for patients with chest wall deformities. We combine the latest surgical techniques, including the advanced Nuss procedure with ZipFix technology, with comprehensive pre- and postoperative care to achieve optimal outcomes for our patients.
Contact Neumark Lung & Chest Surgery Centre today to speak with our expert team about your treatment options.
Pectus excavatum can affect both physical and emotional well-being. In more severe cases, it may compress the heart and lungs, leading to shortness of breath, fatigue, chest discomfort and reduced exercise capacity. Many people also experience self-esteem or body image concerns, particularly during adolescence.
Yes, pectus excavatum pain can cause chest tightness, especially during exercise, deep breathing or poor posture. The pain may result from pressure on the heart or lungs, or muscle strain due to the chest wall deformity. It is more common in teens during growth spurts and in adults with rigid chest structures. If pain affects your daily life, a specialist assessment may help determine if treatment or surgery is needed.
While pectus excavatum cannot be prevented, surgery is a long-term solution. The Nuss procedure, used for correction, provides lasting improvement in chest shape, breathing and confidence. Once the bar is removed, the corrected chest contour is usually permanent.
In very mild cases, it may seem to improve as a child grows. However, most cases persist or worsen during puberty. A specialist consultation and imaging, such as a chest X-ray or CT scan, can help determine if surgery is indicated.
Surgery may be recommended if the condition causes physical symptoms or significantly affects quality of life. This could include difficulty breathing, chest pain, reduced stamina or poor posture. For others, emotional or psychological distress may be a valid reason to consider surgical correction.
Surgery is often performed during early adolescence when the chest wall is still flexible and recovery is quicker. However, many adults also undergo successful correction with modern techniques. The timing depends on individual anatomy, symptoms and overall health.
Pectus excavatum surgery, especially when performed by experienced thoracic surgeons, is generally safe and well tolerated. Like all surgeries, there are potential risks including bleeding, infection or bar displacement, but serious complications are uncommon. Most patients recover well and have excellent outcomes.
DISCLAIMER: The information provided on this website is for general informational purposes only and is not intended as a substitute for professional medical advice, diagnosis, or treatment. The use of this website does not create a doctor-patient relationship and no medical advice should be inferred or assumed. It is the user’s sole responsibility to seek the advice of their healthcare professionals for any medical concerns they may have and the user should not disregard, or delay, prompt medical advice for any such condition.
Neumark Lung and Chest Surgery Centre benefits from the expertise of a multidisciplinary team led by Dr Harish Mithiran, senior consulting thoracic surgeon at Gleneagles Hospital and Mt Alvernia Hospital.
Neumark is a lung and chest specialist centre with access to leading treatment modalities to achieve the best possible outcomes for lung disease and preventative patient screening.
Our foremost priority is to treat your condition as effectively as possible. Schedule a private consultation today; complete the form below, call, +65 6908 2145; WhatsApp, +65 9726 2485; or email, info@neumarksurgery.com.
Gleneagles Medical Centre
6 Napier Road
#02-09 Gleneagles Medical Centre
Singapore 258499
Mount Alvernia Hospital
820 Thomson Road
#06-07 Medical Centre A
Singapore 574623