Hemoptysis, or coughing up blood, is an understandably alarming symptom. It’s a sign that there might be a severe underlying issue or condition, such as lung cancer. In cases of hemoptysis in lung cancer, it’s not just an incidental finding but a major clinical event that needs to be treated urgently. Whether it’s streaks of blood in your sputum or a life-threatening massive haemorrhage, hemoptysis has big implications for diagnosis, prognosis and treatment.
What is Hemoptysis?
Hemoptysis, the medical term for coughing up blood or blood-stained mucus from the lungs or airways, is a symptom that can occur from many underlying conditions. These include lung cancer, tuberculosis, bronchiectasis, and a pulmonary embolism. Hemoptysis affects about 1-2% of the general population, but the incidence can vary depending on the underlying cause and population demographics.
Hemoptysis is divided into three categories: minor, moderate and massive. Minor hemoptysis involves small amounts of blood mixed with sputum. Moderate hemoptysis involves more blood, and massive hemoptysis involves more than 200 ml of blood in 24 hours. In the event of massive hemoptysis, airway obstruction and asphyxiation are immediate and life-threatening concerns and require prompt and decisive intervention.
Recognising and treating hemoptysis early is crucial, especially in lung cancer, where it can be an early sign or a complication of the disease.

The Hemoptysis Lung Cancer Connection
In about 27% of cases, hemoptysis is a symptom of lung cancer and is an important sign at various stages of the disease. For some, it’s the first sign that leads to diagnosis. For others, it’s a complication during treatment, or the late stage of the disease. Beyond the physical impact, hemoptysis also causes emotional and psychological distress, so expert care and reassurance are needed.
As the lungs have a dual blood supply, hemoptysis is often common in cases of lung cancer, where the arteries in the lungs are compromised. Chronic bronchitis and lung disease contribute to hemoptysis through inflammation and vascular changes. Tumours can invade blood vessels, causing bleeding. Systemic factors like anticoagulation therapy, infections, inflammation, and vascular abnormalities that may coexist with malignancy also increase the risk of bleeding.
Pulmonary circulation is low-pressure and is for gas exchange, while the bronchial arteries are high-pressure and supply the lung’s framework. In malignancy-associated hemoptysis, the bronchial arteries are usually the source, although pulmonary artery involvement, albeit less common, adds another layer of complexity to management. Bronchial artery embolisation has become a key intervention for life-threatening hemoptysis and has changed the way hemoptysis is treated.

Causes of Hemoptysis
There are many causes of hemoptysis, though the cause varies by geography and healthcare setting. Globally, tuberculosis is the most common cause. In developed countries, acute respiratory infections, COPD, lung cancer and bronchiectasis are also common causes. Less common causes include pulmonary embolisms, iatrogenic pulmonary artery ruptures and lung abscesses.
In some patients, despite thorough investigation, the cause of hemoptysis remains unknown, and the symptom resolves within 6 months. Understanding the broad differential diagnosis of hemoptysis is important for healthcare providers to ensure accurate diagnosis and management.

The Role of Early Detection with Chest CT
For many patients, hemoptysis is the first sign of lung cancer. Recognising and acting on this symptom can be life-saving as early detection is the key to effective treatment. Diagnostic evaluation starts with a complete history, physical examination, advanced imaging and interventional techniques.
- A CT scan with angiographic enhancement is the gold standard for diagnosing hemoptysis. It localises the bleeding site while providing details on tumour size, location and vascular involvement. Chest CT, especially multidetector CT (MDCT), is also important in diagnosing hemoptysis causes. It helps identify underlying conditions and minimises unexplained cases.
- Bronchoscopy for hemoptysis is a key part of evaluating the condition because it allows direct visualisation of the airways, identification of the bleeding site, and, in some cases, therapeutic intervention.
- Blood tests, including coagulation profiles and inflammatory markers, help identify the contributing factors and guide treatment. Initial complementary tests should include clinical laboratory tests, especially complete blood counts, to assess the severity of bleeding and the patient’s overall condition.

Types of Lung Cancer: NSCLC and SCLC
Lung cancer, which is commonly associated with hemoptysis, is broadly classified into two main types: non-small cell lung cancer (NSCLC) and small cell lung cancer (SCLC). NSCLC accounts for about 85% of all lung cancers and includes subtypes such as adenocarcinoma, squamous cell carcinoma, and large cell carcinoma. Each subtype has its own characteristics and treatment approach. SCLC, which is about 15% of lung cancer, is aggressive and fast-growing.
Both types of lung cancer can cause hemoptysis through tumour invasion of blood vessels or erosion of the bronchial arteries. Knowing the type of lung cancer is important to determine the best treatment for hemoptysis.
Risk Factors for Lung Cancer: Smoking, Carcinogens, Family History
Several risk factors contribute to lung cancer and, thereby, hemoptysis. Smoking is the most common, accounting for 80-90% of all lung cancer deaths and is the leading cause of the disease.
Other risk factors include exposure to asbestos, radon and arsenic. A family history of lung cancer is also associated with increased risk. Chronic obstructive pulmonary disease (COPD) and pulmonary fibrosis are also associated with higher risks of lung cancer. Identifying and managing these risk factors is key to lung cancer prevention and early detection, which can improve outcomes for patients with symptoms like hemoptysis.
A Multidisciplinary Approach to Hemoptysis Management for Lung Cancer
Management of hemoptysis in lung cancer requires an individualised approach that balances immediate stabilisation with long-term disease control. Both the severity and underlying cause of the bleeding can vary and are important factors in designing the treatment approach.
Mild cases may respond to conservative measures such as antibiotics for infections or adjustment of anticoagulation therapy. But more severe bleeding requires advanced interventions, such as:
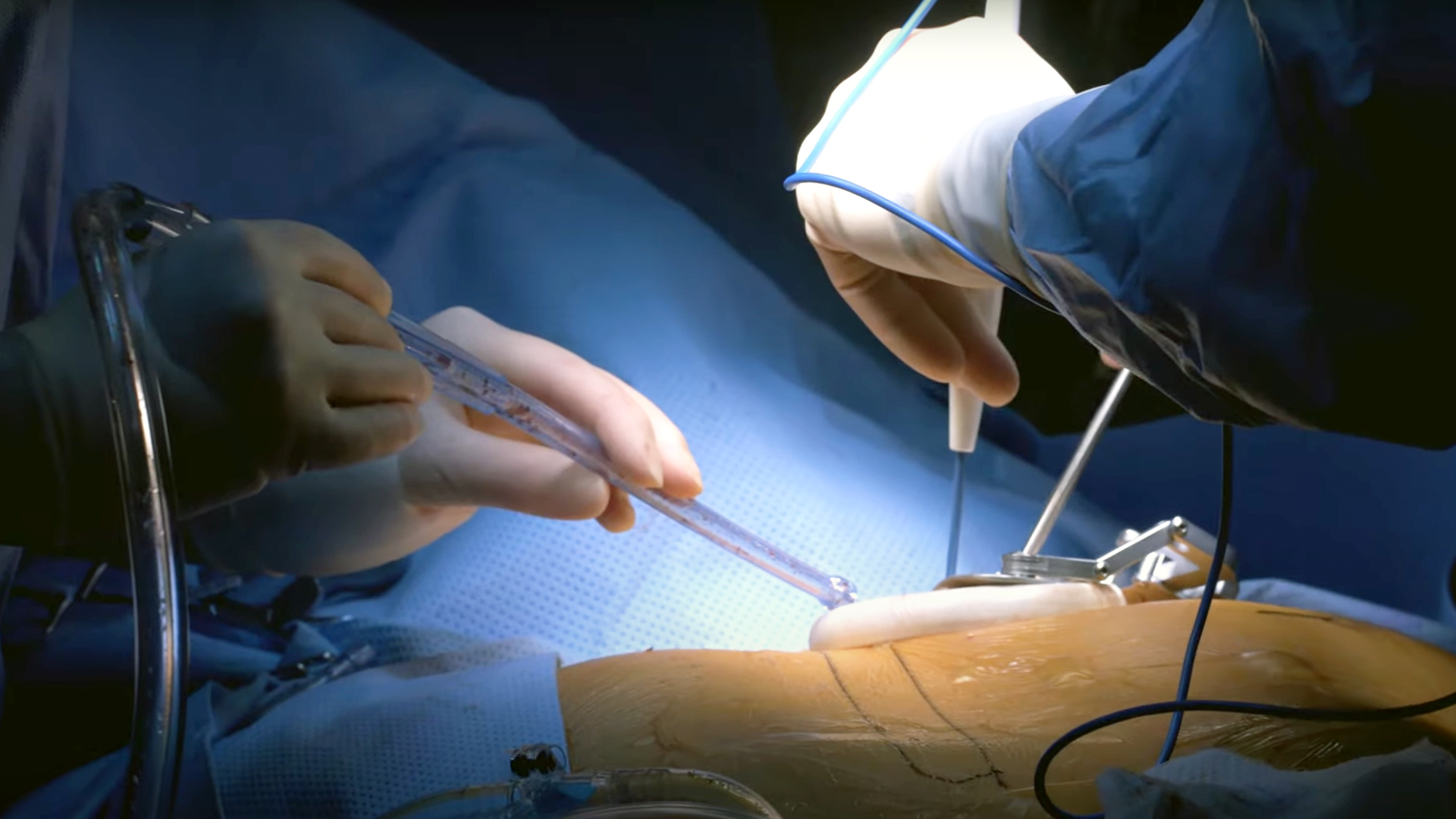
- Bronchoscopic: Bronchoscopy is both diagnostic and therapeutic. Options include electrocautery, laser therapy and placement of endobronchial blockers or stents to control bleeding.
- Arterial Embolization: Often the first line treatment for massive hemoptysis, arterial embolisation involves selectively occluding the bleeding bronchial arteries using embolic agents. Performed by interventional radiologists, this minimally invasive procedure has high success rates and low complication risk. It is particularly effective in managing recurrent hemoptysis and reducing the risk of further bleeding episodes.
- Surgical Intervention: In cases of recurrent or refractory hemoptysis, thoracic surgery may be needed. Procedures such as lobectomy or pneumonectomy aim to remove the source of bleeding while preserving as much healthy lung tissue as possible.
The Expertise Neumark Lung & Chest Surgery Centre Offers
Hemoptysis, if managed early, can lead to a diagnosis of lung cancer at a stage where curative treatments are still possible. Early identification and treatment of conditions like lung abscesses, which can cause hemoptysis, is critical in preventing complications. Low-dose CT scans, regular screening for high-risk individuals, and advances in targeted therapy have changed the landscape of lung cancer care and given hope to many patients.
Call Neumark Lung & Chest Surgery Centre today to book a consultation or a lung cancer screening. Early detection and specialised care can save your life!

