Bronchogenic lung cancer remains one of the most prevalent and lethal malignancies worldwide, with a devastating impact on patients and their families, despite the remarkable advancements in its diagnosis and treatment over the past few decades.
Bronchogenic lung cancer refers to malignant neoplasms that arise from the epithelium of the bronchial tree. It encompasses several subtypes, primarily categorised into non-small cell lung cancer (NSCLC) and small cell lung cancer (SCLC). NSCLC accounts for approximately 80-85% of all lung cancers and includes adenocarcinoma, squamous cell carcinoma, and large cell carcinoma. SCLC, while less common, is known for its aggressive behaviour and rapid growth.
The global burden of bronchogenic lung cancer is staggering. According to the World Health Organisation, lung cancer is the leading cause of cancer-related deaths worldwide, with an estimated 1.8 million deaths in 2022 alone. While smoking remains the primary risk factor, accounting for about 80-90% of cases, other factors such as environmental pollutants, occupational exposures, and genetic predisposition also play significant roles.
The development of bronchogenic lung cancer is a complex, multistep process involving accumulation of genetic and epigenetic alterations. These changes lead to the activation of oncogenes and inactivation of tumour suppressor genes, resulting in uncontrolled cell proliferation and survival.

Recent advances in molecular biology have changed our understanding of lung cancer. Identifying driver mutations in genes such as EGFR, ALK, ROS1, and BRAF has paved the way for targeted therapies, significantly improving outcomes for subsets of patients with advanced disease.
Clinical presentation and diagnosis
The clinical presentation of bronchogenic carcinoma can be insidious, with many patients remaining asymptomatic until the disease is advanced. Common symptoms include a persistent cough, hemoptysis, dyspnea, chest pain, and systemic symptoms like weight loss and fatigue. Symptoms present in patients related to local invasion or distant metastases, such as hoarseness due to recurrent laryngeal nerve involvement or neurological symptoms from brain metastases.
Diagnosis typically involves a combination of imaging studies and tissue biopsy. Chest radiography is often the initial imaging modality, but computed tomography (CT) provides more detailed information about the primary tumour and potential metastases. Positron emission tomography (PET) has become an invaluable tool for staging, offering insights into the tumour’s anatomical and metabolic characteristics.
Tissue diagnosis is crucial and can be obtained through various methods:
- Bronchoscopy with endobronchial biopsy or transbronchial needle aspiration
- CT-guided percutaneous needle biopsy
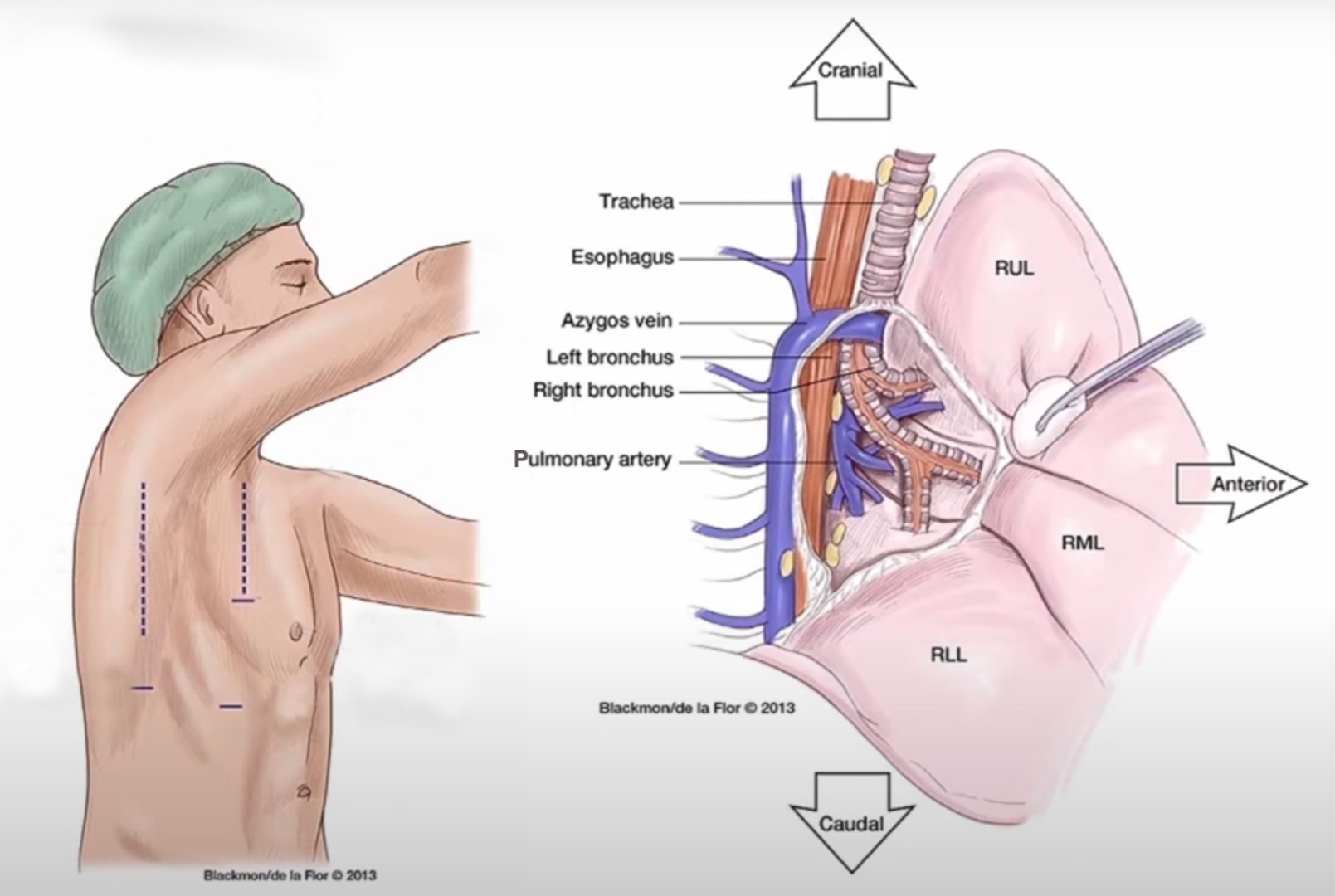
- Video-assisted thoracoscopic surgery (VATS) biopsy
- Mediastinoscopy for lymph node sampling
The choice of biopsy technique depends on the tumour’s location, size, and the patient’s overall condition. VATS is particularly useful for peripheral lesions, offering excellent diagnostic yield with minimal invasiveness.
Bronchogenic lung cancer treatment approaches by stage
Treatment approaches vary based on the stage of the disease and the patient’s overall health:
Early-Stage NSCLC (Stages I and II)
Surgical resection remains the gold standard for early-stage NSCLC. VATS lobectomy, for instance, has become increasingly popular due to its minimally invasive nature and excellent oncological outcomes. For patients who are not surgical candidates, stereotactic body radiation therapy (SBRT) offers a highly effective alternative.
Locally Advanced NSCLC (Stage III)
Management of stage III disease often involves a multimodality approach. Depending on the specific presentation, treatment may include a combination of chemotherapy, radiation therapy and surgery. The integration of immunotherapy in this setting has shown promising results in recent clinical trials.
Advanced NSCLC (Stage IV)
Systemic therapy is the mainstay of treatment for patients with metastatic disease. Targeted therapies and immunotherapy have transformed the landscape of advanced NSCLC treatment. Patients with actionable mutations (e.g. EGFR, ALK) can benefit from specific tyrosine kinase inhibitors, while immune checkpoint inhibitors have shown remarkable efficacy in a subset of patients.
Small Cell Lung Cancer
SCLC is typically treated with chemotherapy, often combined with radiation therapy for limited-stage disease. While surgery is rarely indicated in SCLC, surgical resection may play a role in very early-stage disease, though such cases are uncommon.
Early detection of bronchogenic lung cancer remains essential
Despite significant advances, bronchogenic carcinoma continues to pose substantial challenges. Early detection remains a critical issue, with many patients still presenting with advanced disease. Low-dose CT screening for high-risk individuals has shown promise in reducing lung cancer mortality, but implementation and adherence remain challenging.
The evolution of lung cancer management has moved from a largely palliative approach to one that offers real hope for long-term survival, even in advanced stages. Early detection, personalised treatment approaches, and continued research into the disease’s molecular underpinnings are key to improving outcomes. By combining surgical expertise with cutting-edge medical therapies and emerging technologies, we can significantly reduce the burden of this devastating disease in the coming years.

