Nonseminomatous germ cell tumours, or NSGCTs, can also form outside the testes or ovaries, known as extragonadal germ cell tumours. These can appear in different places, including the mediastinum, the middle part of the chest close to the lungs. Their location or spread to the lung tissue could indirectly affect lung health.
The outlook and treatment for extragonadal NSGCTs depend on multiple factors, such as if it’s seminoma or nonseminoma, how big it is, where it’s located, what the blood marker levels are, how far it’s spread, and how it first responds to treatment. These details help your medical treatment team tackle your condition and personalise a guiding treatment approach.
Nonseminomatous Tumour Treatment
To treat nonseminomatous tumours, doctors often start with a combination chemotherapy regimen known as BEP, including bleomycin, etoposide and cisplatin. This is a common first step in the treatment plan. After chemotherapy, if there are still parts of the tumour left (referred to as residual masses), surgery to remove these areas in the chest might be the next step.
It’s important to understand that if the cancer relapses after this initial chemotherapy treatment, the outlook for the patient is generally not as hopeful. Further treatment options and decisions would depend on the specifics of the relapse, including where the cancer has spread and how it responds to additional treatments.
Mediastinal nonseminomas, which are tumours found in the chest area, get extra focus because of where they’re located and the specific challenges they bring, like the chance they might lead to hematologic neoplasia, a type of blood cancer.
It’s been found that with the right treatment approach tailored to the individual’s specific situation, about half of the people with these tumours can expect to survive. This suggests the importance of having customised treatment plans for each patient’s needs and circumstances.
Extrapleural Pneumonectomy for Early Stage Malignant Mesothelioma
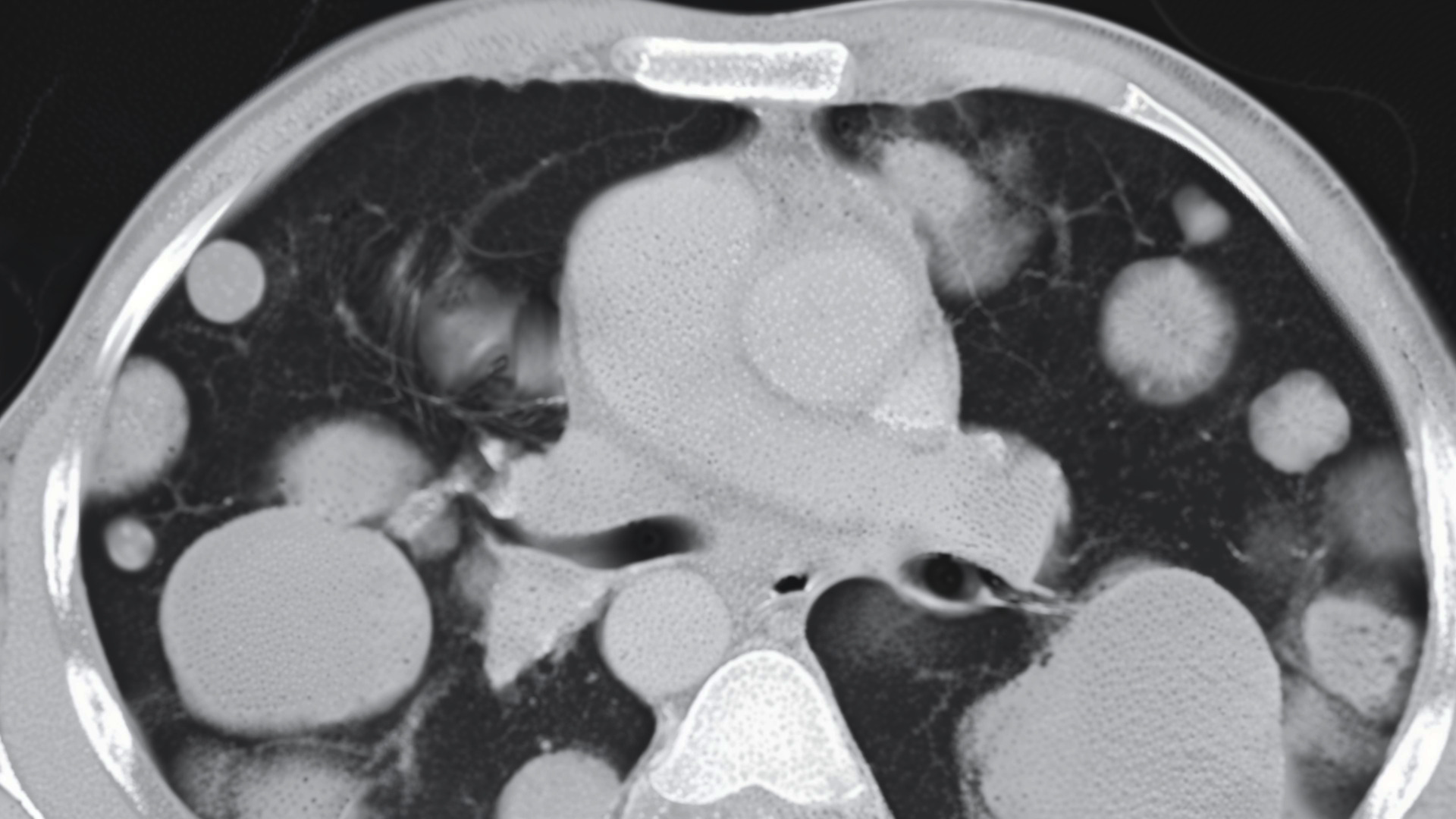
An extrapleural pneumonectomy (EPP) is a major and complex surgical procedure, most often employed in treating malignant mesothelioma in its early stages. This operation is not taken lightly, as it involves the removal of an entire lung, along with portions of the surrounding diaphragm, pleura (the lining around the lungs), and sometimes part of the pericardium (the lining around the heart). Such a drastic measure aims to eliminate cancer before it has a chance to spread to lymph nodes or other tissues and organs, thereby potentially improving outcomes for patients diagnosed at an early stage of this aggressive disease.
The procedure requires expertise and is performed in specialised medical centres by experienced thoracic surgeons.
Due to its invasiveness, patients must be carefully selected based on their overall health, the specific characteristics of their cancer, and their ability to withstand both the surgery and the recovery period that follows. The hope is that, by removing the tumour entirely, along with the lung and other affected areas, the spread of the disease can be halted or slowed, offering a better prognosis for the patient.
Given the seriousness of the operation and the recovery process, patients considering an extrapleural pneumonectomy should discuss all potential risks and benefits with their healthcare team. This includes understanding the possible complications, the likelihood of improvement in their condition, and what life after surgery may look like, including the impact on their breathing and overall quality of life.
EPP is often a complex operation that involves removing the diseased lung along with parts of the diaphragm, the pleura, and part of the pericardium. This procedure is aimed at patients with early-stage mesothelioma because it requires the patient to be in otherwise good health with adequate heart and lung function, considering the significant load increase on the heart and the remaining lung after the surgery.
Recovery from EPP is extensive and may require a hospital stay of one to two weeks, followed by a significant recovery period at home. Patients need careful monitoring due to the potential for serious complications, and the procedure carries a certain mortality risk. However, EPP may significantly impact life expectancy and quality of life, particularly when combined with other treatments like chemotherapy and radiation .
Though aimed at improving survival and controlling the disease, this operation carries significant risks, including internal bleeding, respiratory failure, and the possibility of cancer recurrence.
New Advancements in Minimally-Invasive Surgeries
With the advancements in minimally invasive surgeries like Video-Assisted Thoracoscopic Surgery (VATS) and Robotic-Assisted Thoracic Surgery (RATS), options for lung cancer surgery post-neoadjuvant therapy have expanded. These methods offer similar survival and complication rates to traditional open resection but with benefits like reduced blood loss and shorter hospital stays.

Schedule a Consultation
While EPP offers extended survival and possibly a cure in certain cases, eligibility for the surgery requires a thorough evaluation, including biopsies, imaging scans, and tests to assess lung function and heart health. These tests help determine if the cancer has spread and if the patient’s body can withstand the removal of a lung and subsequent treatments.
The choice between RATS and VATS is influenced by each patient’s specific condition, the surgical team’s expertise, and the available technology. RATS provides advantages in complex resections. Both approaches signify progress in treating lung cancer, including conditions requiring extrapleural pneumonectomy, focusing on patient outcomes and quality of life improvement.
Patients facing this severe and complex operation must thoroughly discuss potential benefits and risks with their surgical team to make an informed treatment decision, reflecting the evolving landscape of surgical options for lung cancer treatment.
Neumark Lung & Chest Surgery Centre specialises in thoracic care and focuses on delivering optimal patient outcomes for a healthier future. If you are concerned about a recent lung cancer diagnosis, arrange a consultation with our lung specialist today.

