
When breathing becomes more difficult or you start to experience unexplained chest discomfort, it is easy to attribute it to fatigue or a passing cold. However, persistent shortness of breath or chest heaviness can signal a more serious condition, such as pleural effusion. This condition involves an abnormal accumulation of fluid between the layers of tissue that line the lungs and chest cavity. While it may sound alarming, pleural effusion is manageable and, with proper treatment, many patients regain normal lung function and comfort.
The lungs are encased in a protective lining called the pleura, which consists of two layers: the visceral pleura, which is attached to the lungs, and the parietal pleura, which is attached to the chest wall. The pleural surfaces, the visceral and parietal pleura, are in close contact, facilitating smooth lung movement during respiration.
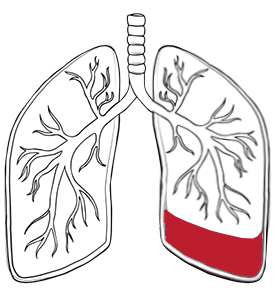
The pleural space normally contains approximately 30 millilitres of fluid, which serves as a natural lubricant, allowing the lungs to move smoothly during breathing. This delicate balance ensures comfortable respiration and optimal lung function. When this system becomes disrupted, such as by increased pressure in the pulmonary circulation or decreased blood protein levels, fluid can leak into the pleural space. Excess fluid can accumulate, creating pressure that restricts lung expansion and causes considerable discomfort, requiring swift diagnosis and action.
Pleural effusions are classified into distinct categories based on the fluid’s composition and underlying causes to help determine the most appropriate treatment approach:

Symptoms of pleural effusion vary considerably depending on the volume of fluid accumulation and the underlying cause. The greater the build-up of fluid, the more likely symptoms will be noticeable. Many patients initially dismiss early symptoms as common respiratory complaints, delaying crucial diagnosis and treatment.
Common symptoms include progressive shortness of breath, particularly during physical activity or when lying flat. Chest pain often presents as a sharp pain that worsens with deep breathing or coughing. A persistent dry cough may develop as the body attempts to clear a perceived obstruction.
In extreme cases, a person can have up to four litres of excess fluid in the chest, making breathing extremely uncomfortable. Patients frequently describe feeling as though something is pressing against their chest, preventing them from fully expanding their lungs.
Additional symptoms may include fever, particularly when the infection causes the effusion, and general fatigue resulting from compromised oxygen exchange. Some individuals experience reduced exercise tolerance and difficulty sleeping due to breathing difficulties when lying down. A prompt medical evaluation is essential for an accurate diagnosis and effective treatment.

Pleural effusion is not a condition in itself but a symptom of an underlying disease. Among the most common causes of pleural effusion are:
Some people have more than one of the causes above. The most common causes include heart failure, which accounts for a significant proportion of transudative effusions. When the heart cannot pump effectively, fluid backs up into the lungs and surrounding tissues, sometimes resulting in pulmonary oedema.
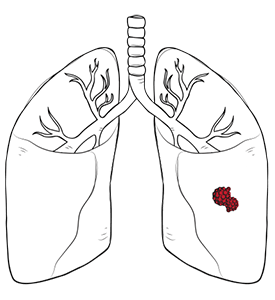
Cancer represents another major cause, either through direct tumour involvement or as a side effect of treatment. Malignant pleural effusion often indicates advanced disease and requires specialised oncological management alongside treatment for pleural effusion.
Infections, particularly pneumonia and tuberculosis, can trigger inflammatory responses leading to fluid accumulation. Liver disease, kidney failure, and autoimmune conditions such as inflammatory bowel disease also contribute to pleural effusion. Lung injury, ovarian hyperstimulation syndrome and oesophageal rupture are additional potential causes that should be considered in the differential diagnosis.
Less common examples of what can cause a pleural effusion include pulmonary embolism, medication reactions and trauma. Identifying the cause of pleural effusion is essential for management. Identifying the underlying cause is crucial for developing an effective treatment strategy and preventing recurrence.

Doctors use physical exams and imaging to diagnose pleural effusion. Chest radiographs are often the first step in identifying pleural effusion, as they can reveal the presence of fluid in the pleural space. The radiographs help detect fluid levels, the meniscus sign, and blunting of the costophrenic angles. Further imaging, such as an ultrasound or a CT scan, may be used to determine the exact volume and location of the effusion.
A key step in diagnosis is thoracentesis, a procedure where a needle is inserted into the pleural space to withdraw fluid. This sample is then analysed to determine whether the effusion is transudative or exudative, which helps identify the underlying cause and guide treatment. Advanced diagnostic techniques may include pleural biopsy when initial fluid analysis proves inconclusive.
There are several treatment options for pleural effusion, depending on the underlying cause and severity. In many cases, especially with smaller effusions, conservative treatment and medication may be sufficient. Diuretics can be used for effusions caused by heart failure, while antibiotics may be prescribed for those resulting from infections.
When fluid continues to build or causes significant discomfort, draining fluid from the chest cavity becomes a key step in management. This can be done through repeated thoracentesis or by inserting chest tubes to remove fluid over time. Chest tubes are commonly used in the management of pleural diseases, especially when larger volumes need to be drained or when ongoing drainage is required. For recurrent or complex cases, surgical intervention may be necessary.

At Neumark, video-assisted thoracic surgery (VATS) is a minimally invasive option for pleural effusions that need more than simple drainage. This approach is used to diagnose the cause of the fluid, perform pleurodesis to prevent recurrence, clear complex or loculated fluid, and release trapped lung caused by scarring. Through small incisions, surgeons can visualise the chest cavity and address multiple issues in a single procedure. Patients often experience less pain, shorter hospital stays, and a quicker recovery compared to traditional open surgery.

In certain complex cases, a traditional thoracotomy may still be necessary. This open surgical approach enables more extensive procedures, such as decortication (the removal of fibrous tissue that restricts lung expansion) or a full exploration of the pleural cavity in cases of difficult infections or malignancies. The decision between VATS and thoracotomy is made carefully based on the patient’s specific condition and overall health.

Pleural effusions can sometimes lead to serious complications if not managed promptly and effectively. One of the most significant risks is respiratory failure, which can occur if excess fluid in the pleural space severely restricts lung expansion. In rare cases, large or rapidly accumulating pleural effusions may also put pressure on the heart, leading to a life-threatening condition known as cardiac tamponade. Another potential complication is empyema, where infection causes pus to collect in the pleural cavity, often requiring urgent intervention.
The prognosis for pleural effusions varies widely and is closely linked to the underlying cause and the speed with which treatment is initiated. For example, malignant pleural effusions, often associated with advanced lung cancer or metastatic disease, tend to have a poorer outlook, with median survival rates typically ranging from four to six months. In contrast, transudative pleural effusions resulting from conditions like congestive heart failure or a pulmonary embolism can have a much better prognosis, especially when the underlying heart failure or clot is treated effectively.
Accurate diagnosis of pleural effusion is crucial for determining the most effective course of action and predicting outcomes. Pleural fluid analysis, including measurements of pleural fluid protein and lactate dehydrogenase (LDH), helps differentiate between complicated vs uncomplicated pleural effusions, guiding further management. In some cases, additional procedures such as pleural biopsy or the placement of an indwelling pleural catheter may be necessary to both diagnose and treat persistent or complicated pleural effusions. When infection or malignancy is involved, more aggressive treatments like chest tube drainage and targeted antibiotics or cancer therapies may be required.
Ultimately, early recognition and comprehensive evaluation are key to improving prognosis and reducing the risk of complications in patients with pleural effusions.

Recovery time varies significantly based on the chosen treatment approach. After thoracentesis, patients may need to take it easy for two days, whilst VATS requires a few days of hospitalisation. Traditional thoracotomy typically requires approximately one week of hospital stay.
Postoperative care includes pain management, respiratory therapy and a gradual progression of activity. Patients receive detailed instructions on wound care, activity restrictions and signs of complications that require immediate medical attention.
Long-term management requires regular follow-up appointments to monitor for the redevelopment of effusion and assess the effectiveness of treatment.

Preventing the recurrence of pleural effusion largely depends on addressing the underlying cause. For example, in malignant effusions, repeated fluid accumulation can be managed through the use of indwelling pleural catheters or chemical pleurodesis. For infectious causes, complete treatment of the infection is crucial.
Lifestyle adjustments may also play a role, particularly in managing heart or kidney conditions that can lead to recurrent fluid retention. Our team at Neumark offers long-term follow-up and monitoring, ensuring patients receive comprehensive care even after the initial treatment.

Yes, in some cases. While draining the fluid often relieves symptoms, a persistent or infected effusion can lead to a condition called a trapped lung. This occurs when a thick, fibrous peel forms on the lung’s surface, preventing it from fully re-expanding. If left untreated, this can cause permanent loss of lung function and lead to chronic breathlessness, requiring a surgical procedure called decortication to remove the peel.
A pleural effusion is almost always a symptom, not the primary disease. It’s the body’s response to an underlying issue, much like a fever. The fluid can accumulate from various conditions, including heart failure, pneumonia, kidney disease, or cancer. The most important part of our diagnosis is not just draining the fluid, but meticulously analysing it to pinpoint the root cause so we can treat the right problem.
Not necessarily. A small amount of fluid can be a sign of a serious issue, such as a malignant tumour, while a large effusion might be a response to a benign condition, like heart failure. The fluid’s characteristics, such as its colour, protein content, or the presence of specific cells, are far more important than its volume in determining the cause and severity.
Yes, it can. If the underlying cause of the effusion is not fully treated, the fluid will likely return. For example, if the effusion is caused by cancer, it will continue to re-accumulate until the cancer itself is managed. For recurrent effusions, we may discuss procedures to prevent the fluid from returning, such as a pleurodesis, where we seal the pleural space, or placing an indwelling pleural catheter for long-term drainage at home.
It’s a subtle but crucial difference. Diagnostic drainage involves removing a small amount of fluid for laboratory analysis to find the cause. Therapeutic drainage involves removing a large amount of fluid to relieve a patient’s symptoms, such as severe shortness of breath. Often, both are done simultaneously, but the goals are different. Your surgeon will ensure that the drained fluid is sent for all necessary tests to secure a definitive diagnosis, rather than just providing symptomatic relief.
DISCLAIMER: The information provided on this website is for general informational purposes only and is not intended as a substitute for professional medical advice, diagnosis, or treatment. The use of this website does not create a doctor-patient relationship and no medical advice should be inferred or assumed. It is the user’s sole responsibility to seek the advice of their healthcare professionals for any medical concerns they may have and the user should not disregard, or delay, prompt medical advice for any such condition.
Neumark Lung and Chest Surgery Centre benefits from the expertise of a multidisciplinary team led by Dr Harish Mithiran, senior consulting thoracic surgeon at Gleneagles Hospital and Mt Alvernia Hospital.
Neumark is a lung and chest specialist centre with access to leading treatment modalities to achieve the best possible outcomes for lung disease and preventative patient screening.
Our foremost priority is to treat your condition as effectively as possible. Schedule a private consultation today; complete the form below, call, +65 6908 2145; WhatsApp, +65 9726 2485; or email, info@neumarksurgery.com.
Gleneagles Medical Centre
6 Napier Road
#02-09 Gleneagles Medical Centre
Singapore 258499
Mount Alvernia Hospital
820 Thomson Road
#06-07 Medical Centre A
Singapore 574623