
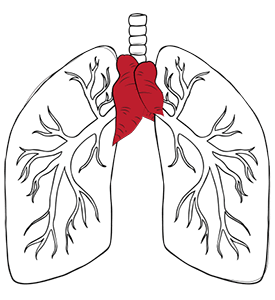
Thymoma is one of the toughest diagnoses in thoracic medicine, but with the proper treatment, many patients do very well. This rare cancer starts in the thymus gland, a small but vital organ behind the breastbone that helps develop your immune system during childhood and adolescence.
What makes thymoma tricky is its association with autoimmune conditions, most notably myasthenia gravis, which affects almost half of all thymoma patients. This means that thymoma treatment often requires addressing both the cancer and the immune system complications.
The good news is that when caught early, thymoma cancer responds very well to treatment. Complete removal is the ideal scenario, especially for localised disease. However, for advanced cases, a carefully coordinated approach involving surgery, radiation, and chemotherapy is necessary. This multidisciplinary approach has improved survival rates over the past two decades, and many patients return to whole, active lives.
Early detection makes all the difference in thymoma outcomes. Unlike many cancers, thymoma doesn’t have a screening protocol, so awareness of symptoms and prompt medical evaluation is key. The combination of expert surgical intervention, targeted therapies, and comprehensive supportive care is the foundation of thymoma treatment in Singapore’s top hospitals.
Diagnosing thymoma can be tricky, as thymoma symptoms often mimic more common conditions. Many patients initially experience chest discomfort, persistent cough or unexplained shortness of breath. These symptoms develop gradually as the growing tumour presses on surrounding structures in the chest cavity. Additionally, there are no definitive causes of thymoma, making it harder to predict, as there are no known risk factors.
What sets thymoma apart from other chest conditions is its association with paraneoplastic syndromes. Myasthenia gravis, which affects about 40 to 50% of thymoma patients, causes muscle weakness that worsens with activity and improves with rest. Some tell-tale signs of thymoma include drooping eyelids, difficulty swallowing, or weakness in the arms and legs, which may appear before any chest symptoms emerge.
Other associated conditions include pure red cell aplasia, where the body stops producing enough red blood cells, and hypogammaglobulinaemia, which increases susceptibility to infection. These immune system complications often provide the first clue that leads to thymoma diagnosis.
The diagnostic journey starts with chest imaging. CT scans show the characteristic anterior mediastinal mass, while MRI provides detailed information on the tumour’s relationship to surrounding structures, such as the heart, major blood vessels, and lungs. Careful evaluation of the primary tumour, mediastinal pleura, and lymph nodes during imaging and staging is crucial for guiding accurate diagnosis and treatment planning. These imaging studies will determine if the tumour is contained within the thymus or has spread to nearby tissues.
A definitive diagnosis typically requires tissue sampling, which is usually obtained through a CT-guided biopsy or surgical sampling.

Clinical and pathological predictors, such as tumour size, histology, and the presence of metastatic thymoma, are essential for prognosis and treatment planning.
Stage I thymomas are completely encapsulated within the thymus gland with no invasion into surrounding structures. These early-stage tumours have the best prognosis when completely removed surgically. Most patients with Stage I disease remain disease-free long-term after a complete thymectomy.
Stage II disease is characterised by invasion into the thymic capsule or surrounding mediastinal fat, but without compromising vital structures, such as the pericardium or great vessels. While still curable with surgery, these cases may benefit from adjuvant radiation therapy to reduce recurrence risk.
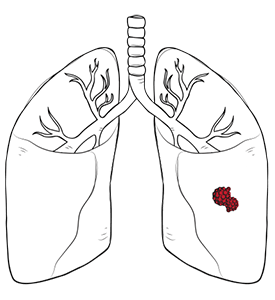
Stage III thymomas invade neighbouring structures, such as the pericardium, lung, or major blood vessels. These cases present greater surgical challenges and require more extensive operations. Complete resection is the goal, but achieving clear margins becomes more difficult.
Stage IV disease is subdivided into IVa (pleural or pericardial implants) and IVb (distant metastases to liver, bones or other organs). These advanced thymomas require multimodal therapy, often starting with chemotherapy to shrink the tumour before surgical resection.
Complete resection when possible improves survival rates across all stages, making surgical expertise crucial in thymoma treatment.
Thymoma treatment is individualised and tailored to tumour stage, histologic type, and patient factors. The primary goals are complete tumour removal, symptom relief, management of associated autoimmune conditions and optimisation of long-term quality of life.
Treatment planning requires consideration of whether you are dealing with a true thymoma or the more aggressive thymic carcinoma. Thymomas generally respond better to treatment and have a better prognosis, while thymic carcinomas behave more aggressively and may require more intensive therapy and multimodal treatment.
Patient factors also influence treatment selection. Age, overall health status, presence of myasthenia gravis, and personal preferences all factor into developing the best treatment plan.
Complete thymectomy is the cornerstone of thymoma treatment for resectable disease. This involves removing the entire thymus gland along with the tumour, surrounding fat, and any involved adjacent structures. The extent of surgery depends on tumour size, location and degree of invasion.
For smaller early-stage tumours, minimally invasive techniques offer significant advantages. Video-Assisted Thoracoscopic Surgery (VATS) and Robotic-Assisted Thoracoscopic Surgery (RATS) enable the complete removal of tumours through small incisions. These approaches result in less pain, shorter hospital stays, and faster recoveries compared to open surgery. Larger or more invasive tumours may require open thymectomy through a median sternotomy (breastbone incision). This approach offers excellent exposure for complex cases that require the removal of invaded structures or the reconstruction of major blood vessels.
The surgical goal is to achieve complete resection with clear margins. Studies consistently show that complete removal provides the best long-term outcome with significantly lower recurrence rate and better survival. Even in advanced cases, aggressive surgical resection combined with other therapies can achieve excellent results.

Radiation therapy plays an essential adjuvant role in thymoma treatment, especially after incomplete resection or in advanced-stage disease, to reduce the risk of local recurrence. External beam radiation therapy targets any remaining tumour cells while sparing surrounding healthy tissues.
Postoperative radiation is planned in consultation with a radiation oncologist to optimise local control and tailor treatment to individual patient factors. Modern radiation techniques, including intensity-modulated radiation therapy (IMRT), allow precise dose delivery while minimising exposure to the heart, lungs and other critical structures.
For patients with inoperable disease due to extensive invasion or medical contraindication to surgery, radiation therapy can be used as primary treatment. While not as effective as complete surgical removal, radiation can provide excellent local control and symptom relief in carefully selected cases.

Chemotherapy has multiple roles in comprehensive thymoma treatment. Neoadjuvant chemotherapy given before surgery can shrink large tumours to facilitate complete resection by targeting and destroying tumour cells. This is particularly useful for bulky Stage III thymomas or cases where initial assessment suggests borderline resectability.
Induction chemotherapy is used in advanced or unresectable thymomas to shrink tumours and improve surgical outcomes. Adjuvant chemotherapy given after surgery targets any remaining microscopic disease. This is typically reserved for high-risk cases with incomplete resection or aggressive histologic features, to reduce the risk of recurrence. Common chemotherapy regimens combine platinum-based drugs with other agents like doxorubicin or etoposide. Etoposide combination chemotherapy is commonly used for advanced or metastatic cases as part of multimodal treatment.
For metastatic or recurrent disease, systemic chemotherapy is the primary treatment option. Thymomas generally respond well to chemotherapy; however, thymic carcinomas may require more aggressive treatment regimens.

Follow-up care is essential for anyone treated for thymoma and thymic carcinoma, as these rare cancers can recur even after initial therapy. Regular appointments with your healthcare provider allow for close monitoring of your condition, early detection of any recurrence, and prompt management of new or persistent symptoms.
Imaging studies such as CT scans or PET scans are commonly used to track changes in the tumour or identify new growths. Blood tests can also provide insight into immune system health and detect potential complications. Long-term effects of treatment, particularly radiation therapy, need to be monitored and managed. Patients should be aware of potential late side effects and collaborate with their care team to address any concerns that may arise over time.
Overall health and well-being are a key part of follow-up care. This includes managing any ongoing symptoms, staying up to date with recommended screenings and seeking support for emotional and psychological needs. With vigilant follow-up and access to evolving treatment options, patients with thymomas can expect improved outcomes and a better quality of life.

Neumark Lung & Chest Surgery Centre brings exceptional expertise to thymoma management under the leadership of Dr Harish Mithiran, who specialises in advanced minimally invasive thoracic surgery techniques. Our centre’s focus on precision surgery, using both VATS and RATS, ensures optimal outcomes with reduced complications and faster recoveries.
We cover every aspect of thymoma care from initial diagnosis to long-term follow-up. We work closely with oncology colleagues to ensure seamless coordination of multimodal therapy when required. The combination of surgical expertise, advanced technology and personalised care creates an environment where patients receive the highest standard of treatment.
Operating at both Gleneagles Hospital and Mount Alvernia Hospital provides access to full inpatient support services, including intensive care capabilities when needed. This infrastructure ensures that even the most complex cases receive appropriate support throughout their treatment journey.
If you or a loved one has a thymoma diagnosis, don’t navigate this journey alone. The team at Neumark is here to provide the personalised thymoma treatment you deserve. Contact us today at +65 6908 2145 or +65 9726 2485.
Yes, surgery is almost always the first and best line of thymoma treatment, even for the earliest stages. Unlike some other cancers that can be managed with observation or chemotherapy initially, complete surgical removal offers the only chance for a cure and prevents the tumour from advancing to a more invasive stage. The decision to operate is usually straightforward, as removal is vital to confirm the diagnosis and prevent future spread.
Non-invasive types like Type A and AB often do not require any further treatment following complete surgical removal. However, more aggressive sub-types like B2 or B3 carry a higher risk of recurrence. In these cases, particularly if the surgeon notes the tumour invaded neighbouring structures, post-operative radiotherapy is commonly recommended to sterilise the area and significantly reduce the chance of the cancer returning.
Surgery often improves, but does not reliably cure, the related myasthenia gravis (MG). MG is an autoimmune condition, and removing the thymus (thymectomy) can induce long-term remission in many patients, even if the thymus gland itself does not harbour a tumour. When a thymoma is present, its removal is still mandatory. In fact, many patients with thymoma see an improvement in their MG symptoms post-surgery, though they will usually require continued medical management by a neurologist.
Minimally invasive approaches like VATS (Video-Assisted Thoracic Surgery) or RATS (Robotic-Assisted Thoracic Surgery) can still be safely used for larger thymoma treatment, provided the surgeon can achieve R0 resection (complete removal with clear margins). If the tumour is large but shows no signs of invading major blood vessels or the lung, a robotic approach offers superior visualisation and precision for meticulous dissection. The decision hinges on the ability to achieve a complete, clean removal, not simply the tumour’s size.
Yes, absolutely. Recurrent thymoma often appears locally (in the chest) and usually grows slowly. If the recurrence is limited to one or two accessible sites, surgery is often the preferred strategy again, even after a previous operation or radiotherapy. The surgeon’s aim is once more to remove all gross disease. The patient’s overall health and previous treatment history will determine if surgery is followed by further chemotherapy or radiotherapy.
DISCLAIMER: The information provided on this website is for general informational purposes only and is not intended as a substitute for professional medical advice, diagnosis, or treatment. The use of this website does not create a doctor-patient relationship and no medical advice should be inferred or assumed. It is the user’s sole responsibility to seek the advice of their healthcare professionals for any medical concerns they may have and the user should not disregard, or delay, prompt medical advice for any such condition.
Neumark Lung and Chest Surgery Centre benefits from the expertise of a multidisciplinary team led by Dr Harish Mithiran, senior consulting thoracic surgeon at Gleneagles Hospital and Mt Alvernia Hospital.
Neumark is a lung and chest specialist centre with access to leading treatment modalities to achieve the best possible outcomes for lung disease and preventative patient screening.
Our foremost priority is to treat your condition as effectively as possible. Schedule a private consultation today; complete the form below, call, +65 6908 2145; WhatsApp, +65 9726 2485; or email, info@neumarksurgery.com.
Gleneagles Medical Centre
6 Napier Road
#02-09 Gleneagles Medical Centre
Singapore 258499
Mount Alvernia Hospital
820 Thomson Road
#06-07 Medical Centre A
Singapore 574623