What Is Empyema Thoracis and When Is Surgery Needed?
Empyema thoracis is a serious infection in the chest in which pus accumulates in the pleural space, the gap between the lung and the inner chest wall. It often starts with pneumonia or a separate lung infection that tracks into the pleura.
Clinicians describe three phases of empyema thoracis as follows:
- In the exudative or ‘oozing’ phase, the infected fluid is thin and may respond to a chest drain and antibiotics.
- The fibrinopurulent phase features thicker pus and noncommunicating pockets, making simple drainage less effective.
- In the organising phase, a tough rind forms on the lung surface. This traps the lung, causing breathlessness, fever, chest pain and fatigue.
Treatment for empyema thoracis depends on the stage. Acting early can change the trajectory, improve prognosis and prevent avoidable complications.
Not every case settles with antibiotics and a drain. Surgery is needed when infection continues despite treatment, when a thick peel forms, when the lung is trapped or partially collapsed, when collections persist or keep returning, or when fibrinolytics don’t work. The longer it is left untreated, the higher the risk of prolonged illness.
If antibiotics and tube drainage haven’t worked, surgical treatment is usually the next step, especially when conservative measures have clearly failed. An operation at the right time removes organised pus, frees the lung and restores more normal breathing mechanics.

What Is Uniportal VATS and Why Use It for Empyema?
Uniportal Video-Assisted Thoracic Surgery (U-VATS) is a minimally invasive approach that utilises a single small incision. Through this one opening, the surgeon inserts a camera and small instruments to both observe and operate inside the chest. The camera magnifies the view, enabling precise dissection and careful removal of infected material.
U-VATS differs from multiport VATS in that it uses a single incision instead of multiple incisions. It’s also different from an open thoracotomy because it avoids an extended cut and rib spreading. For empyema thoracis, these differences matter.
A single incision is usually less painful, and many patients can go home sooner. The visual clarity helps free adhesions and remove the fibrous peel that is holding the lung down. Smaller wounds not only lower the risk of wound complications but also make it easier for patients to get moving, thereby supporting recovery and reducing the likelihood of complications.
However, there are limits to the situations when U-VATS can be used. If the peel is very thick or visibility is poor, the safest course is to convert to an open operation. Even so, for many patients, assisted thoracoscopic surgery reduces the hospital stay compared with an open surgical removal.

Patient Selection and Preoperative Workup
Patients who remain unwell despite receiving antibiotics and a chest tube often improve once the infection is surgically cleared. In frail patients, a tailored minimal-access plan can be safer than prolonged hospitalisation due to infection.
U-VATS is effective for adults and adolescents with stage two or early stage three empyema, particularly when the lung is trapped, an air leak persists, or drainage or fibrinolysis has failed.
Sometimes an open operation is the better option. Extensive adhesions, a dense rind that will not separate safely, a high risk of bleeding, unstable vital signs or significant coexisting illness can all lead to worse outcomes. Experience and judgement are crucial. A prepared team makes intraoperative decisions with the patient’s safety at the centre.
Before surgery, most patients undergo a contrast-enhanced CT scan to define the extent of the disease and to help the surgeon plan the incision. Blood tests check inflammatory markers, nutrition levels and organ function. Sputum and pleural cultures also guide antibiotic selection. Lung function tests are arranged where possible, and an anaesthetic review ensures that single lung ventilation is safe.
All of these elements of preparation are key to ensuring a successful operation, including the right antibiotics, attention to nutrition, reasonable glucose control for those with diabetes and chest physiotherapy.
U-VATS Procedure for Empyema Thoracis
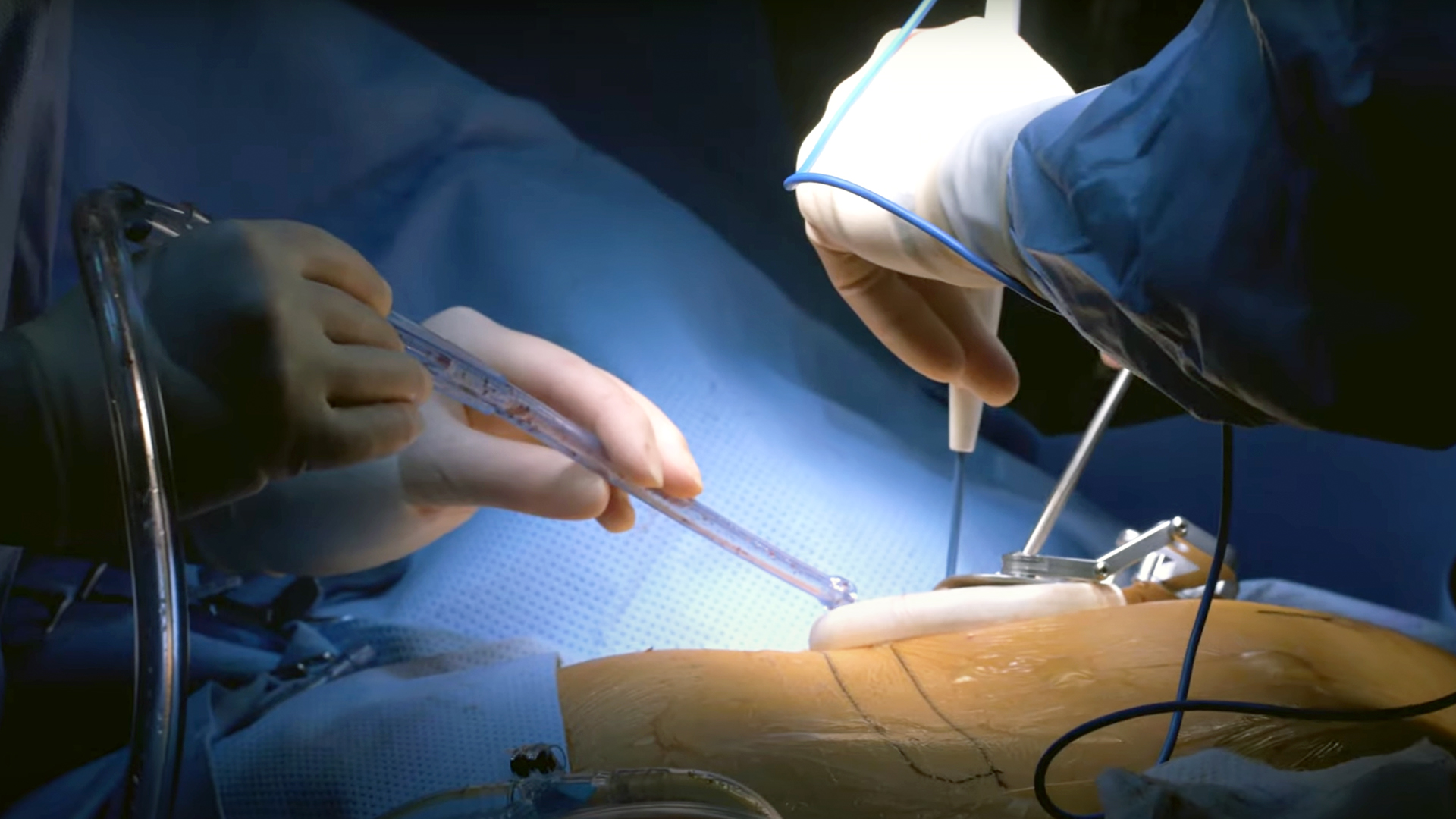
Under general anaesthesia and with one lung ventilated, the patient lies on their side with the affected lung up. The incision is commonly placed at the fifth intercostal space along the midaxillary line, although CT findings guide the exact site.
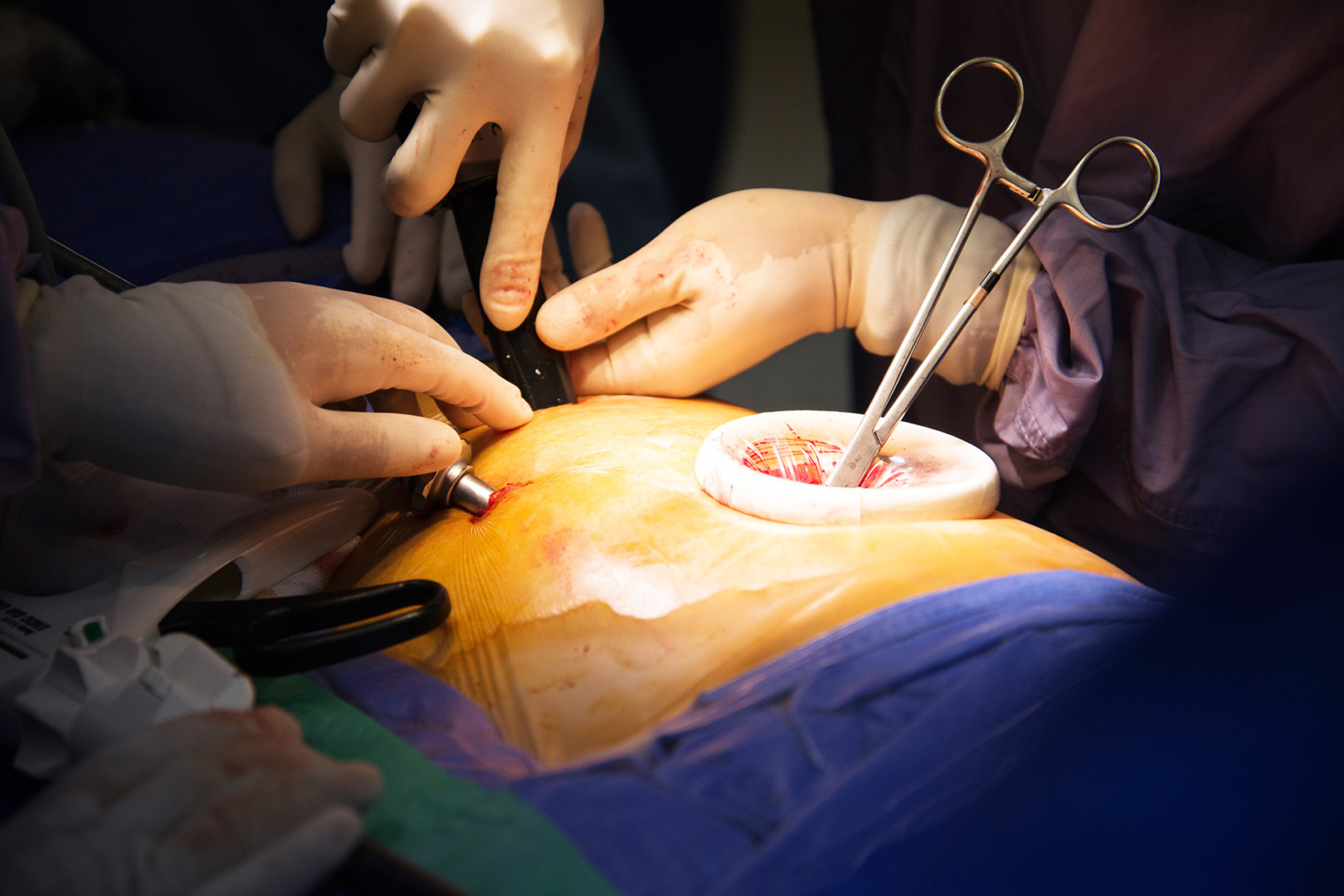
Entry to the pleural space is followed by careful release of adhesions. The surgeon opens the loculations, removes pus, and irrigates the cavity to clear debris. The lung, diaphragm, pericardium and chest wall are protected throughout to avoid injury.
Decortication is a key step in treating empyema thoracis.. The thick fibrous peel is gently lifted from the lung surface to allow full re-expansion. This is often slow and meticulous work, demanding a steady hand. As the rind comes away, the lung fills the chest. Bleeding is controlled, the space is washed, and samples are taken for microbiology and histology.
One or two drains are left in place inside the chest, depending on the findings. These allow residual fluid and air to escape and help keep the lung expanded. If the view is limited or the peel cannot be safely separated, the operation is converted to an open approach.

Risks, Complications and How We Minimise Them
Any operation carries risk. U-VATS for empyema thoracis complications can include a prolonged air leak, bleeding, retained collections, wound infections, recurrence, and occasionally the need for another procedure. These risks are reduced by careful selection, early referral, and a meticulous technique from expert professionals. At Neumark Lung & Chest Surgery Centre, we utilise culture-guided antibiotics, complete decortication when safe, intraoperative imaging when beneficial, and structured post-surgery physiotherapy.
After discharge, patients should seek urgent review if they develop a high fever, worsening breathlessness, chest pain, a persistent cough with sputum production, low oxygen readings, or swelling or discharge at the wound site.
Recovery after U-VATS for Empyema Thoracis
Pain relief is planned to control pain without excessive drowsiness. Drains are monitored and removed when the air leak stops and the fluid output falls. Patients are encouraged to sit up, walk, and practise breathing exercises to prevent collapse of lung segments and aid expansion. Good nutrition supports healing, and physiotherapists coach effective coughing and airway clearance.
At home, you will receive clear instructions on pain management, wound care and activity targets. Many people return to desk work within two to three weeks, with a gradual increase in exercise as comfort and breathing improve. Follow-up includes a wound check, imaging to confirm re-expansion, and an antibiotic plan adjusted to culture results. To prevent recurrence, it is important to complete the course of antibiotics, stop smoking, and manage any underlying lung disease with your respiratory team.

Special Cases for the Surgery
U-VATS is also used in children and adolescents with excellent outcomes. The principles are the same. The focus is on the gentle handling of the chest wall and early recovery. In frail or high-risk adults, strategy and timing become even more important. Shorter, more focused procedures, paired with strong perioperative support, can reduce patient risk.
Empyema may be bilateral or heavily loculated. In these situations, staged operations can be planned. Detailed preoperative imaging will help guide the approach.
Booking Your Consultation
Neumark’s team has extensive experience with U-VATS for empyema thoracis and other complex chest infections. We use an integrated care pathway that combines rapid imaging, microbiology, anaesthetics, physiotherapy, and respiratory medicine. This ensures every patient receives a clear diagnosis and a precise individualised treatment plan.
All surgeries for Neumark are performed at Gleneagles Hospital and Mount Alvernia Hospital, which are fully equipped with inpatient and critical care support. For your consultation, please bring any prior scans, a list of your current medications, details of any allergies, and your culture results. We’ll review them with you and explain all your options, including the role of U-VATS and what to expect during the recovery process. To book an appointment, please contact us directly at Neumark Lung & Chest Surgery Centre.