
When patients ask what a lung lesion is, the most important thing to remember is that it is a description of an abnormal growth, not a diagnosis. A lung lesion is an abnormal area of lung tissue seen on imaging that can occur in one or both lungs. Some pulmonary lesions are due to prior infections like miliary tuberculosis or scarring, and others may be early-stage lung cancer. Lung lesions and lung nodules are often found incidentally during routine or unrelated imaging tests, such as chest X-rays or CT scans. The clinical team’s job is to determine the cause through careful assessment and, where needed, tissue sampling.
Many lung nodules are found by chance during scans for other reasons. Most lung lesions are benign, and distinguishing them from cancerous lung nodules is key to accurate lung cancer diagnosis and treatment planning. A structured approach led by a thoracic specialist helps to separate low-risk findings from those that require treatment.
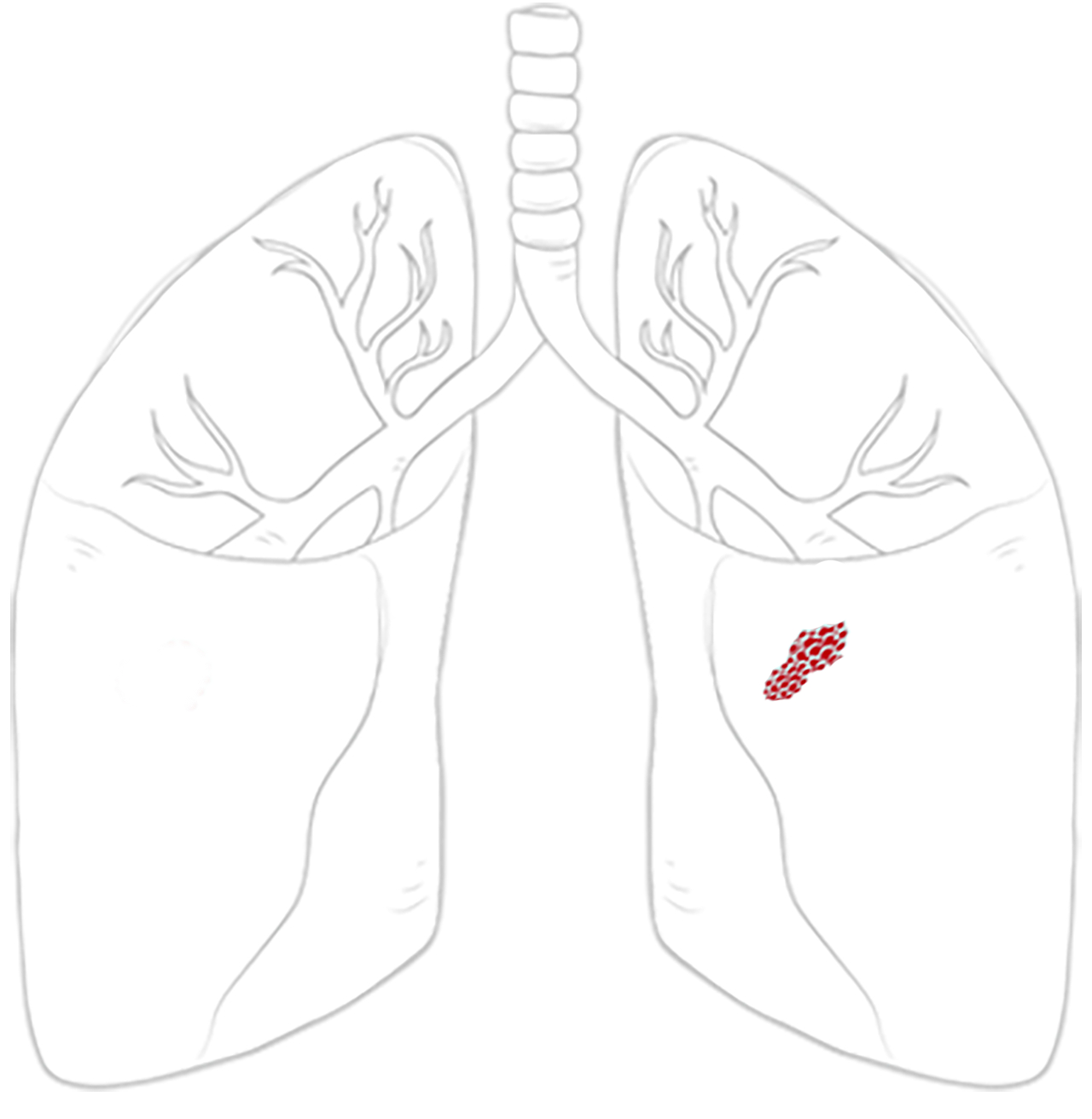
Benign nodules and benign conditions are the most common causes of lung lesions. They may be due to granulomas, hamartomas, chronic inflammation from granulomatous diseases such as rheumatoid arthritis, or scar tissue. Malignant nodules include primary lung cancers, such as small cell lung cancer, and metastases from cancers elsewhere in the body. A malignant nodule may need further evaluation to determine the best treatment.
Risk factors such as smoking (in former smoker patients too), age, family history and exposure to asbestos or air pollution influence how likely a lesion or nodule is to be cancerous. It is important to distinguish lung lesions from other diseases with similar imaging features through differential diagnoses, which may sometimes necessitate a biopsy. Chronic obstructive pulmonary disease can also present with lung abnormalities.
If you are asking what the common symptoms of lung lesions are, the honest answer is that they are often non-specific, which is why imaging tests and clinical review are so necessary. Many do not cause any symptoms. Notably, the absence of symptoms does not rule out a significant finding. When symptoms do occur, they may include a persistent cough, shortness of breath, chest pain or chest discomfort, coughing up blood, wheezing or unexplained weight loss.

The first step after finding a lesion on a lung CT scan is to review the images in detail. A chest X-ray can offer some clues, but a chest CT will provide accurate information about size, shape, density, and location. Chest CT scans are a crucial imaging test for identifying and characterising pulmonary nodules and pulmonary lesions. Radiologists look for features such as smooth or spiculated margins, calcification patterns (e.g., calcium deposits or calcified nodules), growth over time, and whether the nodule is solid, subsolid, or ground-glass in appearance. These CT findings are essential for your specialist to estimate the risk.
A PET scan may be performed after a chest CT to further evaluate the findings. If you are wondering what percentage of pulmonary nodules are likely to be cancerous, there is no definite answer as it depends on the size, appearance and risk profile. In lung cancer screening and in the general population, most incidental pulmonary nodules are benign. Even so, caution is warranted because early detection of lung cancer is difficult, and lung nodules rarely show symptoms initially.

A lung lesion biopsy is often the key to the final diagnosis, and the method is determined by the lesion’s location in the lung parenchyma. Peripheral lesions are usually sampled with CT-guided needle biopsy, while central or airway-adjacent lesions can be reached via bronchoscopy. In some cases, a minor surgical biopsy is the safest option for obtaining sufficient tissue for accurate analysis. Pathology confirms whether the lung lesion is benign or malignant and, if lung cancer, identifies the type.
Only a biopsy can provide a definitive diagnosis of whether a lung lesion is cancerous, as imaging tests alone cannot confirm malignancy. Molecular testing can reveal mutations that guide targeted therapies. A timely lung cancer diagnosis is crucial for improving lung cancer survival rates, reducing patient anxiety, and enabling early detection.

If a solitary pulmonary nodule is small and has low-risk features, a surveillance plan is made. Scans are repeated at defined intervals through yearly lung cancer screenings to detect changes. Patients with particularly high-risk features may require more frequent or intensive monitoring. Stability over two years often suggests that the small nodules or lung lesions are benign. This approach is reassuring for many patients and avoids overtreatment. If the nodule grows or develops concerning features, the plan changes to a biopsy or removal.
If a lung lesion or mass is likely malignant, growing, or causing symptoms, removal may be advised. At Neumark Lung and Chest Surgery Centre, we use minimally invasive techniques for thoracic surgery wherever safe and appropriate.
Video-Assisted Thoracoscopic Surgery (VATS) uses small incisions and a camera to access the chest. Uniportal VATS achieves this through a single incision. Robotic-Assisted Thoracic Surgery (RATS) adds three-dimensional vision and wristed instruments for precise dissection in tight spaces. These approaches allow wedge resection for diagnosis, segmentectomy to remove a segment, or lobectomy when a larger portion is needed in the right lung or upper lobe. Lymph nodes are sampled to stage lung cancer accurately. Patients usually experience less pain and a faster recovery compared to traditional open surgery. Radiation therapy may be considered for patients who are not surgical candidates.
For benign tumours that are growing or causing symptoms, minimally invasive resection is also often the best solution. It confirms the nature of the pulmonary lesions and prevents future complications.

If lung lesions are left unmonitored or untreated, they can sometimes lead to serious complications. Malignant lesions may progress to lung cancer, which can spread to other parts of the body and become life-threatening. Other risks include respiratory failure or persistent symptoms such as chest pain, shortness of breath or unexplained weight loss.
If you have a medical history of lung cancer or other lung diseases, you should be more proactive about regular screenings as a screening test and follow-up. Early medical attention and timely treatment are the best ways to minimise the risks of lung nodules.
When surgery is not advised due to other health conditions after a physical examination, alternatives may include stereotactic body radiotherapy, which delivers focused radiation to a small area, or thermal ablation techniques such as radiofrequency ablation. These methods can control selected larger nodules and are considered on a case-by-case basis after multidisciplinary review. Internal medicine specialists are often involved in evaluating complex cases where surgery is not suitable.

Finding a lesion on a lung CT scan or computed tomography (CT) scan or computed tomography ct does not mean you have lung cancer. Your clinical team will review the features of the nodule, your high-risk factors, and your overall health to assess your situation. They will advise whether monitoring, needle biopsy or removal is best. If surgery is needed, minimally invasive techniques mean most patients recover quickly, often leaving the hospital in a few days.
At Neumark, we focus on accuracy, clear communication, and tailored care. Our team has broad experience in managing lung lesions and pulmonary nodules, from surveillance plans to complex resections using VATS, U-VATS and robotic approaches.
If you have concerns about a lung lesion or lung nodules or want a second opinion, contact Neumark Lung & Chest Surgery Centre. We consult and operate at Gleneagles Hospital and Mount Alvernia Hospital, with full support from the imaging, respiratory, and oncology teams. Call +65 6908 2145 or WhatsApp +65 9726 2485 to book a consultation. Early, expert care matters for lung lesions and lung nodules, whether in a former smoker or as an incidental finding, the size of a green pea.
This decision is based on risk stratification, not guesswork. Your specialist considers a combination of factors, including the lesion’s size, shape, density, location, and whether it has changed over time, along with your age, smoking history, and medical background. A small, smooth lesion in a low-risk patient is often monitored, whereas a lesion with irregular borders, rapid growth, or higher-risk features may require earlier biopsy or removal. The goal is to avoid unnecessary procedures while not missing an early cancer.
Yes, significantly. Lung cancers detected at an early stage, often through investigation of an incidental lung lesion, are more likely to be treatable with curative intent. Early-stage cancers can sometimes be managed with limited surgery, such as a wedge resection or segmentectomy, rather than more extensive treatment. Early detection can also reduce the need for chemotherapy or radiotherapy and is associated with better long-term survival. This is why timely assessment of lung lesions matters, even when you feel well.
Surgery is sometimes advised not because the lesion is definitely cancerous, but because it is indeterminate and potentially risky. In some instances, imaging and biopsy cannot provide a clear answer, or the lesion is in a position where needle biopsy may be unreliable. Minimally invasive surgery can both diagnose and treat the lesion in one step. For many patients, removing a suspicious lesion early is safer than prolonged uncertainty or delayed intervention.
It helps to go into your consultation prepared. Helpful questions include: which features of your lung lesion make it low- or high-risk; the pros and cons of monitoring versus biopsy or surgery in your case; what type of resection would be needed and why, if surgery is recommended; and how the lesion may affect your long-term lung health and follow-up plan. Clear answers to these questions help you make informed decisions and reduce anxiety during what can be an uncertain time.
DISCLAIMER: The information provided on this website is for general informational purposes only and is not intended as a substitute for professional medical advice, diagnosis, or treatment. The use of this website does not create a doctor-patient relationship and no medical advice should be inferred or assumed. It is the user’s sole responsibility to seek the advice of their healthcare professionals for any medical concerns they may have and the user should not disregard, or delay, prompt medical advice for any such condition.
Neumark Lung and Chest Surgery Centre benefits from the expertise of a multidisciplinary team led by Dr Harish Mithiran, senior consulting thoracic surgeon at Gleneagles Hospital and Mt Alvernia Hospital.
Neumark is a lung and chest specialist centre with access to leading treatment modalities to achieve the best possible outcomes for lung disease and preventative patient screening.
Our foremost priority is to treat your condition as effectively as possible. Schedule a private consultation today; complete the form below, call, +65 6908 2145; WhatsApp, +65 9726 2485; or email, info@neumarksurgery.com.
Gleneagles Medical Centre
6 Napier Road
#02-09 Gleneagles Medical Centre
Singapore 258499
Mount Alvernia Hospital
820 Thomson Road
#06-07 Medical Centre A
Singapore 574623