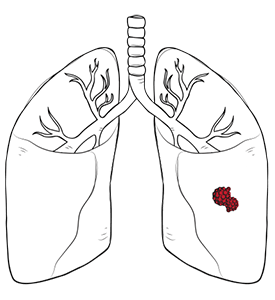

Metastatic lung cancer is a term that describes when cancer spreads from another part of the body to the lungs. While not curable in most cases, early detection and tailored treatment can significantly improve the patient’s quality of life and long-term outcomes.
Metastatic lung cancer occurs when cancer cells break away from a primary tumour elsewhere in the body, travel through the bloodstream or lymphatic system, and lead to secondary tumours in the lungs. The lungs are a common site for metastases, particularly due to their rich blood supply and their role in filtering the blood in the circulatory system.
Cancers that often spread to the lung include breast, colorectal, kidney, prostate and melanoma. Importantly, the tumour in the lungs is the same type of cancer as the source, changing treatment options.
At Neumark Lung & Chest Surgery Centre, we specialise in advanced and minimally invasive surgery, combined with comprehensive medical management, to provide top-quality treatment for patients with metastatic lung cancer.

In many patients, metastatic lung cancer symptoms are mild or even absent in the early stages, which makes detection difficult. Additionally, the symptoms of metastatic lung cancer can vary depending on the location and extent of metastasis, but there are some key signs to look out for:
As these symptoms overlap with those of other respiratory conditions, they are often overlooked. If you have a history of cancer and develop new or unexplained chest symptoms, seek medical evaluation promptly.

The diagnostic process typically begins with imaging tests, such as chest X-rays or CT scans, to identify suspicious nodules or masses. PET-CT scans may be used to determine whether the lesions are metabolically active, thereby allowing distinction between benign and malignant changes.
A biopsy is the gold standard for confirming a metastatic lung cancer diagnosis. Depending on the nodule’s location, this may be performed via bronchoscopy, CT-guided needle biopsy, or surgical biopsy. Once confirmed, staging assessments are done to determine how far the disease has spread and to guide metastatic lung cancer treatment options.
Treatment for metastatic lung cancer depends on the primary cancer type, how far it has spread, and the patient’s overall health. Systemic therapies, such as chemotherapy, targeted drugs, and immunotherapy, form the foundation for controlling tumour growth and improving survival. These treatments can have side effects that affect a patient’s quality of life. It is important to discuss potential side effects and their management with your healthcare team.
Radiation therapy, including advanced techniques like stereotactic body radiotherapy (SBRT), is often used to relieve symptoms like chest pain or breathing difficulties and to control small, well-defined lesions. In selected cases, surgery for metastatic lung cancer, known as pulmonary metastasectomy, can remove lung nodules to relieve symptoms and extend life expectancy.
Lung cancer surgery is usually considered when the primary cancer is controlled, no disease is present outside the lungs, and lung function is strong enough to support recovery. It is very rarely an option when the source of the cancer has not undergone treatment.
Video-Assisted Thoracic Surgery (VATS), commonly known as VATS, is a game-changing approach in treating metastatic lung cancer, utilising small incisions and a camera-guided system to remove lung tissue. This minimally invasive technique offers several advantages over open surgery, including reduced postoperative pain, a shorter hospital stay, and a faster recovery time, allowing patients to return to their daily lives sooner.
VATS is particularly well-suited for resecting solitary or limited metastatic lesions, especially those located peripherally near the lung’s surface. It excels in procedures like wedge resections or segmentectomies, which target metastatic nodules while preserving as much healthy lung tissue as possible, an important consideration for patients with metastatic lung cancer who may face multiple interventions due to recurrent disease.
The magnified, high-definition views provided by VATS allow surgeons to identify and excise lesions with precision, minimising trauma to surrounding tissues. However, its effectiveness is not uniform across cases; for example, it decreases in centrally located metastases or in complex cases that require extensive lymph node dissection or intricate reconstructions, such as sleeve lobectomies. Additionally, VATS can be challenging when multiple metastases are scattered across different lung lobes or when adhesions from prior surgeries complicate access.
For patients with good lung function and limited disease burden, VATS is often the preferred option, especially when rapid recovery is a priority, such as in those undergoing staged resections for metastatic disease.

Robotic-Assisted Thoracic Surgery, or RATS, utilises advanced robotic technology to deliver unparalleled precision, dexterity, and 3D visualisation, enabling surgeons to tackle complex metastatic lung cancer cases with great accuracy, even in confined anatomical spaces. This is particularly useful for challenging cases, such as metastases near critical structures, such as major blood vessels or airways, or when a lobectomy is required for larger or centrally located lesions.
The 3D visuals allow surgeons to pinpoint small or deeply embedded metastases, while its articulated instruments provide access to hard-to-reach areas. Its tremor-free precision is particularly valuable for preserving lung function, a critical consideration for individuals with compromised respiratory capacity or a history of thoracic surgery, where adhesions may complicate access.
For simpler procedures, such as wedge resections of peripheral metastases, the benefits of RATS may not be necessary. However, RATS is often the preferred choice for complex metastatic lung cancer cases, offering a tailored solution that balances oncologic efficacy with the goal of maintaining quality of life through precise, minimally invasive intervention.

Several factors influence whether VATS or RATS is chosen for surgery for metastatic lung cancer:
At Neumark, we work with each patient to weigh these factors and design an approach that balances effectiveness and recovery.

Metastatic lung cancer prognosis for patients with metastatic lung cancer depends on several important factors, including the type of lung cancer, how far it has spread, the patient’s overall health, and how well the cancer responds to treatment. Metastatic lung cancer has a lower 5-year survival rate, roughly ranging from 3% to 9% for those with distant metastases. However, every patient is unique, and advances in lung cancer treatment have helped some patients live longer and have a better quality of life.
Patients with metastatic lung cancer are encouraged to have an open discussion with their doctor about their individual prognosis and what to expect from treatment. Understanding the likely course of the disease can help patients and their families make informed decisions about their care, set realistic goals, and focus on what matters most to them during treatment.

Metastatic lung cancer is a complex condition, but with early diagnosis, personalised treatment, and access to the latest surgical techniques, patients can see significant improvement in both longevity and quality of life.
At Neumark Lung & Chest Surgery Centre, our expertise in VATS and RATS, combined with a multidisciplinary approach, means each patient receives individualised care. We perform all surgical procedures at our affiliated institutions, Gleneagles Hospital and Mount Alvernia Hospital, ensuring access to full inpatient and critical care support.
If you or a loved one has been diagnosed with metastatic lung cancer, contact Neumark Lung Cancer Treatment Centre today. Our team will guide you through diagnosis, treatment, and recovery with care and expertise.
In highly selected cases of oligometastatic disease, surgery may be performed first to achieve a “no evidence of disease” (NED) status. The rationale is that completely removing all known cancer sites, both the primary lung tumour and the single metastasis, may offer the best long-term outcome. Systemic therapy (chemo or immunotherapy) can then be used afterwards to target any residual, microscopic disease and delay recurrence, effectively maximising the chance for prolonged survival.
Yes, it can. Certain targeted therapies, while effective at shrinking the tumour, can sometimes cause changes in the tissue around the tumour, making it tougher or more fibrotic (scarred). This can make the surgical dissection (separating the tumour from surrounding structures) more difficult for the surgeon. Your thoracic surgeon must be aware of your complete systemic therapy history to adjust the operative technique and manage any increased risks.
In cases where a cure is not the primary goal, surgery or a surgical procedure is often used for palliation (relief of symptoms). For example, a surgeon might perform a procedure to stop severe bleeding from the primary tumour or remove a metastasis in the spine that is causing debilitating pain or neurological compromise. The goal here is to provide immediate relief and a rapid improvement in the patient’s quality of life, rather than long-term cancer control.
Yes. A unique aspect of immunotherapy is that its side effects, known as immune-related adverse events (irAEs), can sometimes emerge months or even years after the final treatment dose. These late-onset events, which occur because the immune system remains “revved up,” can manifest as inflammation in the joints, skin, or other organs. Patients must be educated to report any new or unusual symptoms to their care team, regardless of the time elapsed since their last infusion.
The choice between surgical removal (metastasectomy) and Stereotactic Body Radiation Therapy (SBRT) is a highly individualised one, often debated in multidisciplinary tumour boards. Surgery is typically chosen when a complete, R0 removal is feasible and the patient is strong enough to recover from the operation. SBRT, a highly precise, non-invasive form of radiation, is often preferred for patients who are not fit for surgery, or if the metastasis is in a location (like the brain or spine) where surgical access is riskier. Both methods are considered local ablative therapies designed to eliminate the specific site of spread.
DISCLAIMER: The information provided on this website is for general informational purposes only and is not intended as a substitute for professional medical advice, diagnosis, or treatment. The use of this website does not create a doctor-patient relationship and no medical advice should be inferred or assumed. It is the user’s sole responsibility to seek the advice of their healthcare professionals for any medical concerns they may have and the user should not disregard, or delay, prompt medical advice for any such condition.
Neumark Lung and Chest Surgery Centre benefits from the expertise of a multidisciplinary team led by Dr Harish Mithiran, senior consulting thoracic surgeon at Gleneagles Hospital and Mt Alvernia Hospital.
Neumark is a lung and chest specialist centre with access to leading treatment modalities to achieve the best possible outcomes for lung disease and preventative patient screening.
Our foremost priority is to treat your condition as effectively as possible. Schedule a private consultation today; complete the form below, call, +65 6908 2145; WhatsApp, +65 9726 2485; or email, info@neumarksurgery.com.
Gleneagles Medical Centre
6 Napier Road
#02-09 Gleneagles Medical Centre
Singapore 258499
Mount Alvernia Hospital
820 Thomson Road
#06-07 Medical Centre A
Singapore 574623