Diagnosing Lung Nodules Accurately
With lung nodules identified on an estimated 30% to more than 50% of all low-dose computed tomography (CT) scans, and roughly 5% of these being cancerous, accurate diagnosis and treatment can be lifesaving.
The challenge is to accurately diagnose small lung nodules (tiny dots of abnormal tissue) near the outer edge of the lungs (subpleural). Traditional methods, like taking a small tissue sample with a needle guided by imaging (lung biopsy) or even removing a small section of the lung with camera-assisted surgery (thoracoscopic wedge resection), often fall short. They might only sometimes successfully get enough of the suspicious area to make a clear diagnosis.
Shift to Minimally Invasive Lung Biopsy Procedures
Minimally invasive techniques offer a welcome shift from traditional open surgery for patients facing surgery for a lung nodule. One such method is video-assisted thoracoscopic surgery (VATS), which utilises small incisions in the chest wall and relies on a camera for magnified visualisation.
But even with this technology, pinpointing the exact location of a nodule within the lung can be challenging.
Traditional lung cancer biopsy procedures, including needle biopsies, have limitations and risks, such as pneumothorax or ‘lung collapse’. Video-assisted thoracoscopic surgery (VATS) offers a less invasive alternative for diagnosing and removing these nodules. However, locating small, often hard-to-reach nodules can be challenging, even with the advent of novel techniques for lung nodule removal.
“Before the routine use of CT scans, there was a greater reliance on clinical judgement and patient history to guide the management of suspected lung nodules, with invasive diagnostic procedures like thoracotomy being used when necessary but generally avoided due to their risks,” says Dr Harish Mithiran, director of Neumark Surgery and senior consulting thoracic surgeon at Gleneagles Hospital and Mount Alvernia Hospital in Singapore. “The development and refinement of CT-guided technology for lung biopsy have greatly enhanced the ability to detect, diagnose, and treat lung nodules early, often before they become symptomatic, allowing for more timely and less invasive interventions.”
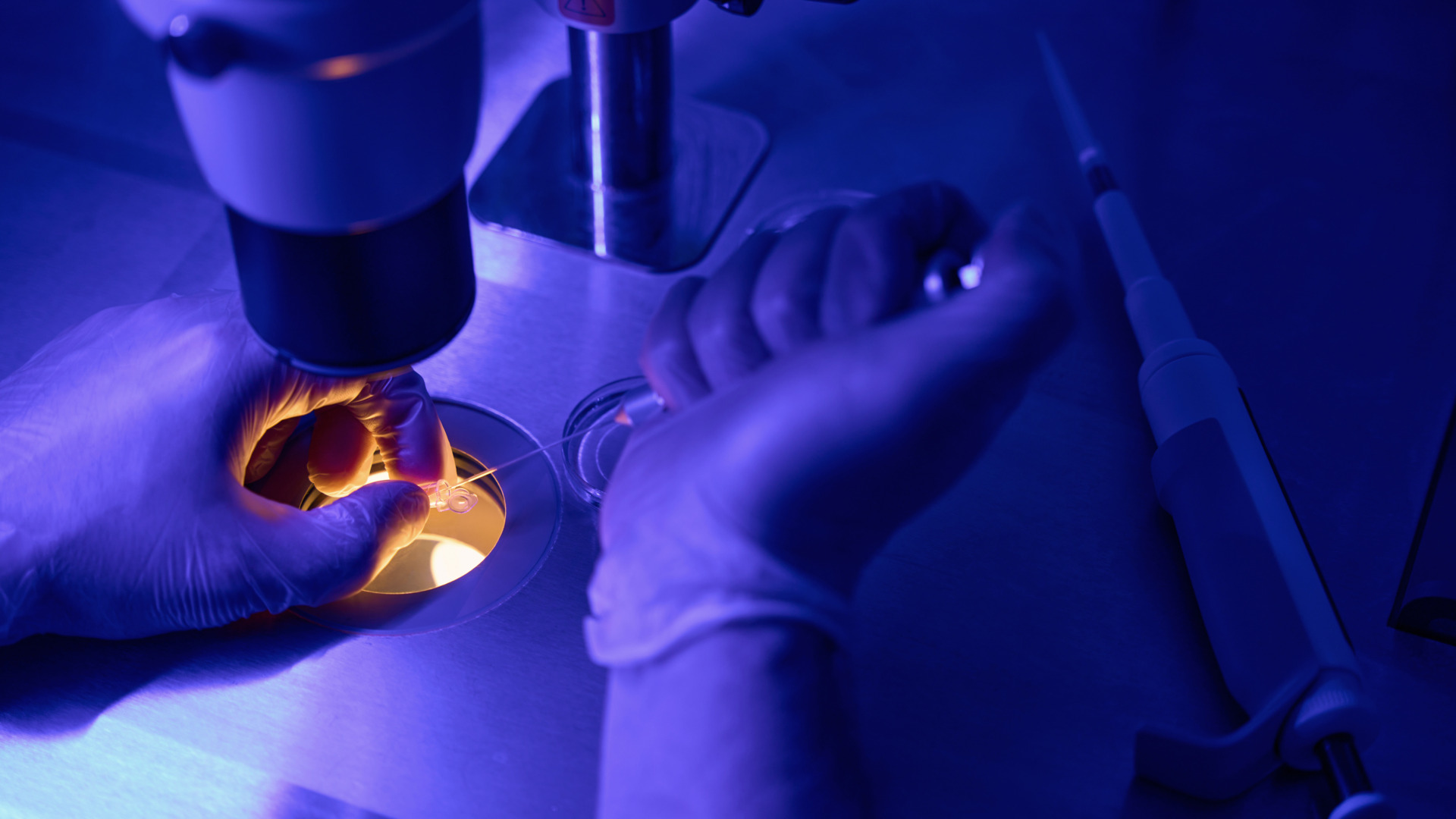
To improve the chances of successfully removing these tricky lung nodules during surgery, the thoracic surgeons at Neumark Surgery use several preoperative localisation techniques daily to improve the accuracy of locating small lung nodules before or during lung biopsies.
Methylene Blue
Methylene blue is injected near the nodule to facilitate nodule identification and removal during surgery. The dye, injected directly into the tissue surrounding the nodule, helps surgeons differentiate the nodule from the surrounding healthy lung tissue, effectively highlighting the otherwise inconspicuous nodule.
This enhanced visualisation gives surgeons a target to remove the nodule, minimising the risk of resecting healthy lung tissues during VATS.
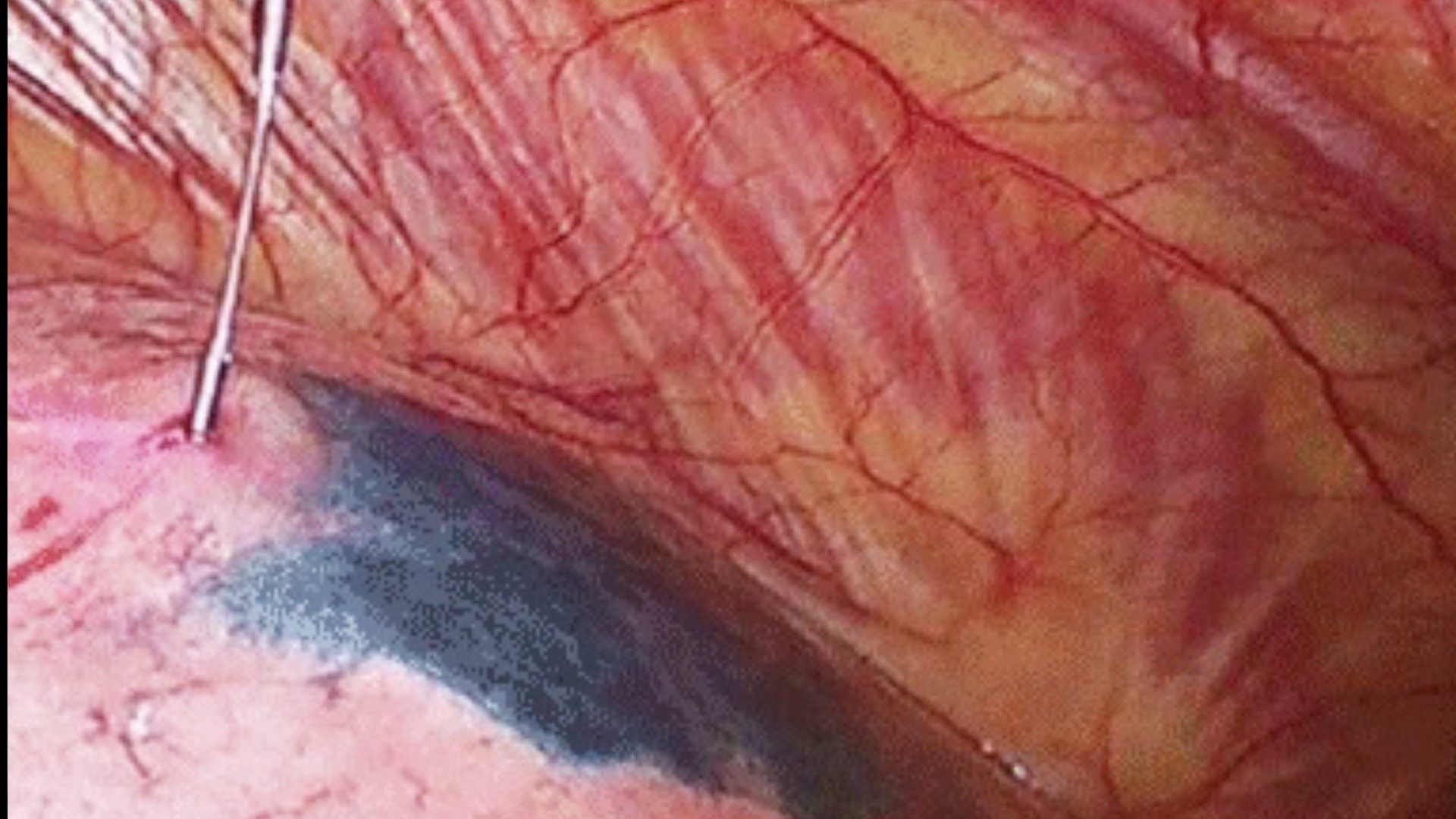
Hookwire
Before surgery, doctors may use a CT-guided lung biopsy procedure with a hookwire at the site of the lung nodule. This technique increases the likelihood of successfully removing difficult-to-see, hard-to-feel nodules. Once the hookwire is in place, it serves as a marker, making it easier for the surgeon to find and remove it during the biopsy.
Microcoil
Microcoil localisation offers another novel way to guide the resection of nonpalpable lung nodules, an alternative to watchful waiting or lobectomy. During the CT-guided lung biopsy procedure, a surgeon inserts a needle into the chest and lung, aiming for the nodule they want to biopsy. This needle contains a soft, fibre-coated platinum wire.
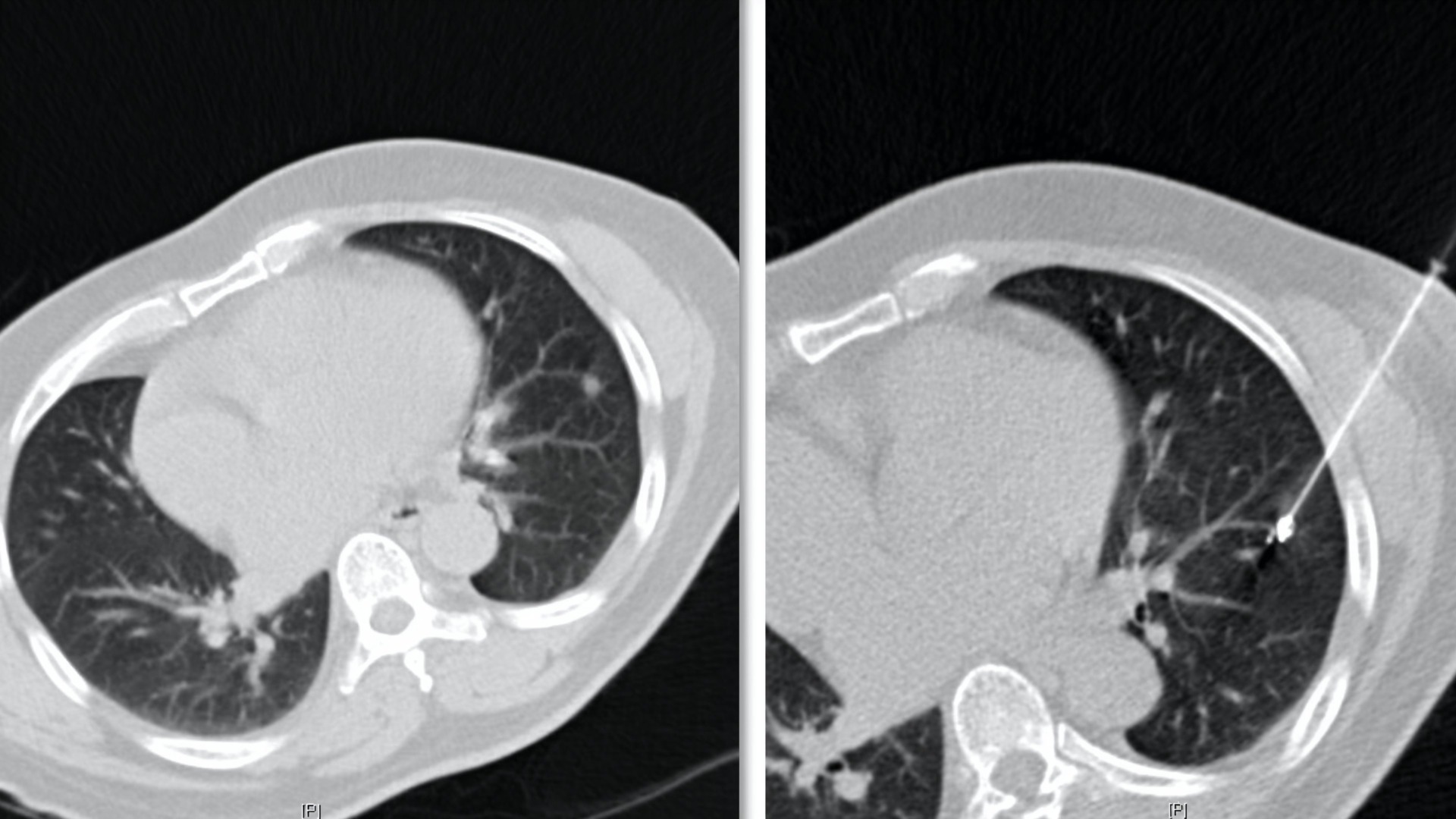
Once the needle reaches the nodule, the wire is pushed out, coiling up within the lung to mark the nodule’s exact location. Then, the needle is slightly pulled back, and the other end of the coil is placed at the lung’s edge, creating a shape like a dumbbell — one end of the coil is attached to the nodule, and the other end is fixed near the lung’s outer layer, connected by the wire. In the next step, a surgeon uses a small camera – a thoracoscope – to see inside the chest and makes a small cut to access the lung. They then deflate the lung to see better and reach the coiled wire.
Following the wire as a guide, the surgeon finds the nodule and removes it with a small amount of surrounding lung tissue.
Indocyanine Green
Indocyanine green, or ICG, enhances the visualisation of small abnormal growths. ICG works intravenously or directly into the lung tissue surrounding the nodule. Once injected, the dye selectively binds to specific proteins and becomes concentrated in certain tissues.
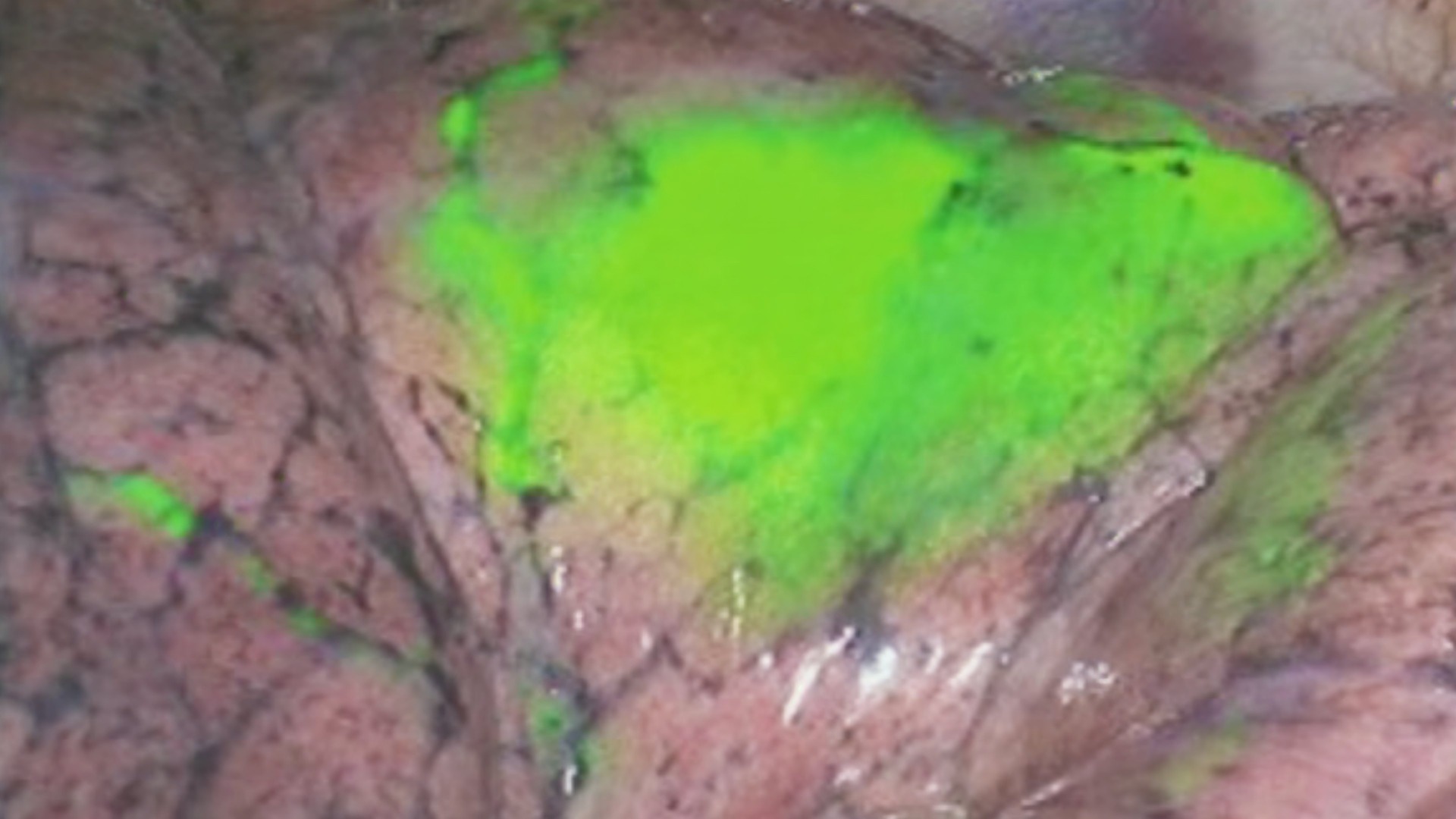
During surgery, surgeons use a special camera equipped with near-infrared light filters. The light highlights the ICG molecules, causing them to fluoresce — essentially ‘glowing’ — under the camera’s view. This fluorescence highlights the nodule against the surrounding healthy lung tissue, making it significantly easier for surgeons to identify and locate.
While metaline blue dye, hook wire localisation, microcoiling and ICG are valuable tools, it’s important to remember that lung biopsy procedures do not diagnose the nodule. Further tests are needed to determine if the growth is cancerous or benign after biopsy.
Each of these localisation techniques has its advantages and drawbacks, and the choice depends on the nodule’s characteristics, the patient’s condition, the surgeon’s recommendations and the equipment used.
VATS Lung Biopsy Recovery Time
Recovery from a VATS lung biopsy typically involves a hospital stay of 1 to 3 days to observe the patient following surgery. Pain, often manageable, is expected, and patients usually resume light activities within a week. However, returning to full normal activities, including work, may require several weeks. Since recovery can vary from person to person, it’s important to discuss with your surgical team what you can expect during your recovery.
Neumark Surgery’s primary aim is to pinpoint and excise potentially malignant nodules with the least risk and discomfort for the patient, thereby enhancing lung cancer treatment results. If you’ve recently discovered you have a lung nodule and are seeking a lung biopsy in Singapore, feel free to schedule a consultation with our surgeons today.