Despite smoking rates lowering in Singapore, lung cancer remains a very common cancer among men and women. It’s the second most deadly cancer for men and the third most deadly for women. That may make it seem like women have less to worry about, but that isn’t the case: lung cancer still makes up 15.7% of cancer mortalities in women.
An alarming study came out late last year that showed that though lung cancer rates are dropping overall, they’re not dropping equally. At a very slight rate, women under 50 are now more likely to contract lung cancer than men. While the exact reasons remain under research, the outcome is clear: women need to be more conscious of lung cancer than ever before. They should opt for early detection over late treatment and attend lung cancer screenings.
Disparities in Female Lung Cancer Patients
Lung cancer used to affect men much more than women. That number is changing as smoking patterns change and the environment shifts. Some research suggests that hormonal influences, particularly oestrogen, may play a role in lung cancer development and progression in women.
Others theorise that, though statistically, men smoke more than women, women have more difficulty kicking the habit. There is no clear answer at the moment as to why exactly lung cancer rates in women are rising. But there is a clear reason why lung cancer mortality rates are worse for women than men.

Women are, unfortunately, often conditioned to treat their pain or discomfort as normal rather than a cause for concern. A study found that women are 20% to 30% more likely to get a misdiagnosis than men as well because of innate biases within the medical fraternity.
Awareness of lung cancer symptoms is critical because the disease often remains undetected until advanced stages. Gender bias can influence diagnostic processes, particularly affecting women who are less frequently offered lung cancer screenings.
“One common scenario involves women presenting with chest tightness or pain dismissed as panic attacks or anxiety”, shared Dr Harish Mithiran, director of Neumark. “It’s only when the patients start coughing up blood that the condition receives attention”.
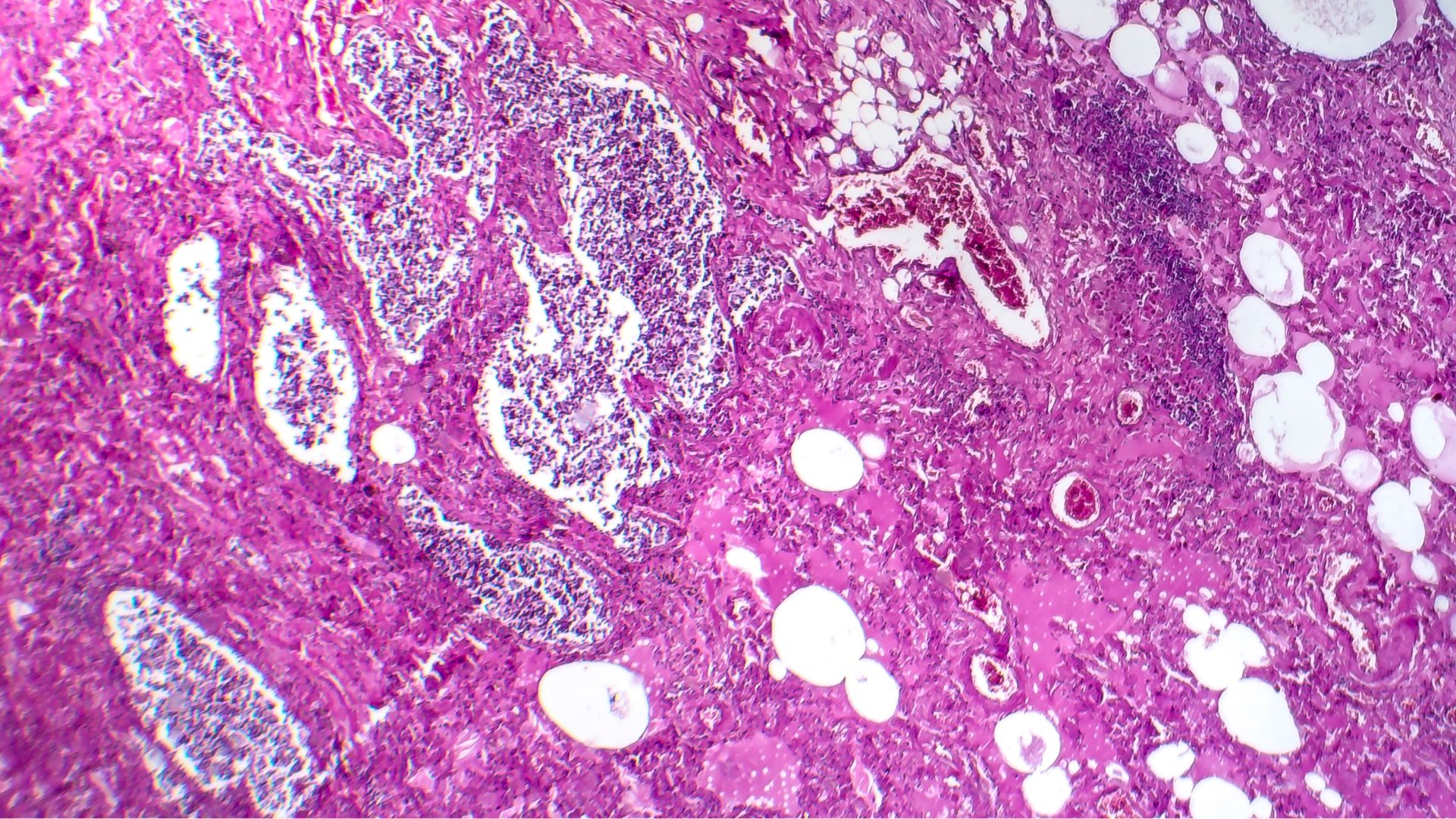
Lung cancer manifests in two primary forms: non-small cell lung caner (NSCLC) and small cell lung cancer (SCLC), each with distinct characteristics and impacts on women. NSCLC, the most prevalent type, includes adenocarcinoma, squamous cell carcinoma and large cell carcinoma. Lung adenocarcinoma is the most common type of lung cancer for women, accounting for 44% of all lung cancer cases. NSCLC tends to progress more slowly, allowing for potentially more treatment options such as surgery, radiation, and targeted therapies. However, NSCLC is often diagnosed at later stages, reducing treatment efficacy.
Conversely, SCLC, though less common, is notorious for its aggressive nature and tendency to metastasize early. This rapid spread often limits treatment options to chemotherapy and radiation, making it more challenging to manage effectively. SCLC occurs most frequently in heavy smokers, which we used to think trended more towards men. As smoking patterns change, SCLC has become a serious risk for women as well.
This late detection is partly due to unrecognised symptoms and underutilised screening. Early indicators include a persistent cough lasting more than six weeks, upper back pain, shortness of breath, unexplained weight loss or a hoarse voice, which can mimic many other common symptoms in today’s age.
To combat these disparities, experts urge women who meet the screening criteria, especially those with a significant family history of lung cancer unrelated to smoking, to advocate for thorough evaluations of their cancer risk.
These factors compound and influence women’s ability to make informed healthcare decisions and to seek timely medical help, affecting diagnosis and treatment outcomes. Regular lung cancer screenings, such as with low-dose CT scans, give patients a fighting chance at accurately detecting the once-deadly disease and the care necessary to ensure cancer remains in remission.
Demographic Shifts Highlight the Need for Early Lung Cancer Screening
During a low-dose CT scan for lung cancer screening, women undergo a quick and painless procedure that uses minimal radiation to create detailed images of the lungs. This scan is effective in detecting early signs of lung cancer, often before symptoms appear, enabling timely and potentially life-saving treatment. The non-invasive process typically takes only a few minutes, making it an essential tool for early detection and treatment outcomes.
Of course, you’re not expected to parse through those results alone. At Neumark, a team of thoracic surgeons, all specialists in lung conditions, will pore over your results to identify any abnormalities. From there, they will decide what makes the most sense moving forward.

Cancer screening tests can help identify potential disease growth and allow Neumark surgeons to remove suspicious tissue during the screening process if abnormalities are found. This can reduce the likelihood of developing recurrent cancer. In some cases, the screening test may require additional follow-up testing. Overall, the best protective plan is to undergo regular cancer screenings.
Even though smoking rates are dropping, lung cancer remains a danger to Singaporeans. In particular, women are at increasing risk as smoking patterns change and biases within medicine persist. The best way to make sure you’re safe is to add regular lung cancer screenings to your annual checkups, especially if you’re in the higher-risk groups, for your peace of mind. That way, a timely intervention can be provided, improving treatment outcomes. Make an appointment for your lung cancer screening today with Neumark Surgery.

