Do not be alarmed if you’ve been told you have a lung neoplasm. Not all of them are cancerous. A lung neoplasm is an abnormal growth of tissue in the lungs. Some are benign and require only observation. Others are malignant, such as lung cancer, which can grow aggressively and spread to other organs and parts of the body.
Lung cancer is the most common cancer in the lungs and the third leading cause of cancer deaths in Singapore for both men and women. It’s important to understand lung neoplasms if you have been diagnosed with them, so that you can understand your treatment.
Primary vs Metastatic Lung Neoplasms
Cancer is treated according to its site of origin. Tumours from other organs can spread to the lung due to their proximity or the pathways of blood and lymphatic circulation. The lung neoplasm definition encompasses primary tumours, which originate in the lung tissue itself, and metastatic tumours, which develop in the breast, colon, or kidney and subsequently spread to the lungs. Importantly, cancers that spread to the lung are not automatically considered ‘lung cancer’.

Types of Lung Neoplasms
Benign lung neoplasms are not cancerous and grow slowly. Many are found incidentally on routine X-rays or CT scans. The most common are:
- Hamartomas account for more than half of benign tumours. These coin-shaped nodules, which are less than 4 cm in diameter, contain cartilage, fat, and muscle.
- Bronchial adenomas develop from mucus glands or ducts in the airway. Carcinoids, a subtype, make up the majority of cases and rarely become malignant.
- Papillomas are rare benign tumours that form in the bronchial tubes. Some are linked to human papillomavirus (HPV).
Benign lung neoplasms can be associated with certain genetic syndromes or environmental exposures that increase the risk of tumour development.
Malignant neoplasms of the lung are cancerous. The main types are:
- Non-small cell lung carcinoma (NSCLC) is the most common, making up 80 to 85% of cases. These include adenocarcinoma, squamous cell carcinoma and large cell carcinoma.
- Small-cell lung cancer (SCLC) is a fast-growing and aggressive cancer that is strongly linked to smoking. Most patients have widespread disease at diagnosis.
- Mesothelioma is a rare cancer of the chest lining, often caused by asbestos exposure.
The type of lung cancer is determined by microscopic examination and is crucial for treatment and prognosis.
Causes and Risk Factors
Smoking is the leading behaviour that causes lung cancer. More importantly, it is the single most significant risk factor for malignant lung neoplasms. Second-hand smoke, asbestos, radon gas and industrial chemicals also increase the risk of lung neoplasms, and the combined effect of these exposures further increases the risk of lung cancer.
Chronic lung conditions like COPD, pulmonary fibrosis and prior tuberculosis also predispose patients to lung neoplasms. Genetic susceptibility plays a role too, with family history, inherited syndromes and ageing all contributing to risk and the likelihood of developing lung cancer.
What Are The Symptoms of Lung Cancer?
Symptoms of lung cancer range from mild to severe. Many patients have no lung neoplasm symptoms at all, with growths only discovered during scans. When present, symptoms may include:
- Persistent or worsening cough
- Coughing up blood
- Shortness of breath or wheezing
- Chest pain or hoarseness
- Recurrent chest infections
- Unexplained weight loss or fatigue
Lung cancer can present with many symptoms, which may vary depending on the stage and type of the disease. It is important for your own health that any persistent respiratory symptoms be evaluated, especially if you have known risk factors.

Diagnosis of Lung Cancer
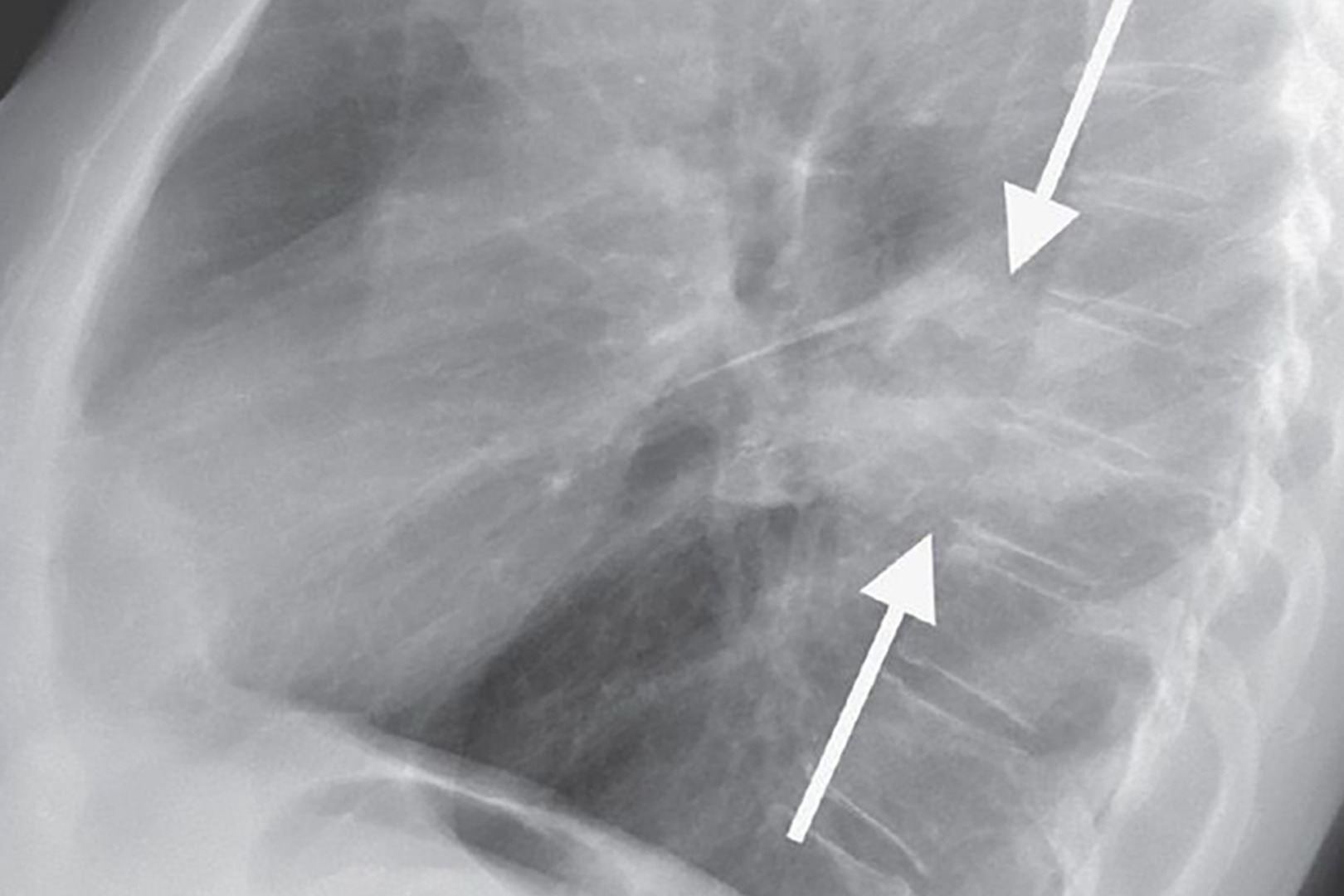
Diagnosis starts with a thorough medical history, physical examination and imaging studies. Chest X-rays are often the first step, but CT scans provide more detailed images and can detect smaller nodules more effectively. PET-CT may be used to see if the tumour is metabolically active in the lung or elsewhere.
Lung function tests help determine overall respiratory health, and blood tests may give clues about general well-being. A biopsy via bronchoscopy, CT-guided needle, or surgical sampling is necessary to confirm if the abnormal tissue is lung cancer. Pathologists examine the tissue under the microscope, and molecular testing may be added to guide targeted therapies.

Staging of Lung Neoplasms
Early-stage lung neoplasms are confined to the lung without nodal involvement or distant spread. These are generally more amenable to surgical removal and have a better prognosis. As the stage advances, especially when lymph nodes are involved or the disease has metastasised to other sites like the brain, liver or bones, treatment becomes more complex and prognosis is poorer.
When a lung neoplasm is malignant, staging is crucial in guiding treatment and prognosis. The most commonly used system is the TNM classification, which evaluates three factors:
- Tumour: size of the neoplasm and if it has invaded surrounding lung tissue
- Nodes: presence or absence of cancer in the nearby lymph nodes
- Metastasis: if the neoplasm has spread beyond the lungs to other organs
Staging not only clarifies the extent of the disease but also ensures that patients receive the most appropriate, targeted therapy. This includes minimally invasive surgery for early-stage tumours, as well as systemic treatments such as chemotherapy, targeted therapy, or immunotherapy for advanced stages of the disease.
Minimally Invasive Surgical Techniques
Treatment depends on whether the neoplasm is benign or malignant. Most benign tumours require only observation with periodic imaging. However, suspicious or symptomatic benign growths may require surgical removal to confirm the diagnosis and prevent malignant transformation.
Malignant tumours often require surgery, one of the mainstays of treatment for early-stage lung cancer, with options including lobectomy, wedge resection, pneumonectomy or more advanced minimally invasive approaches, often combined with chemotherapy or radiation therapy.
At Neumark Lung & Chest Surgery Centre, patients benefit from modern surgical techniques to reduce trauma and speed recovery:
- Video-Assisted Thoracoscopic Surgery (VATS): Small incisions and a camera allow surgeons to remove lung tumours with less pain and a shorter hospital stay.
- Robotic-Assisted Thoracic Surgery (RATS): Using the da Vinci robotic system, surgeons perform precise movements with 3D vision, which is beneficial for complex resections.
- Uniportal VATS (U-VATS): A single incision approach that reduces recovery time even further while maintaining surgical effectiveness.
If surgery is not suitable, Stereotactic Body Radiation Therapy (SBRT), chemotherapy, immunotherapy or targeted therapy may be recommended.
Outcomes depend on whether the tumour is benign or malignant. Benign lung neoplasms have an excellent prognosis and require only monitoring or sometimes resection. For surgically treated early-stage malignant neoplasms, survival rates are high, reaching 80% or more in some cases.

Prevention and Screening
The best prevention is to avoid tobacco. Quitting smoking reduces risk even years after cessation, so it’s never too early to quit smoking. Reducing exposure to industrial carcinogens and maintaining healthy lungs through exercise and vaccinations helps prevent disease. Low-dose CT screening is recommended for high-risk individuals as it focuses on the lung to detect abnormalities early, often leading to earlier detection and better outcomes.

Living with a Lung Neoplasm
A lung neoplasm is not always a cancer diagnosis. Every lung growth warrants expert evaluation. Advances in imaging, precise diagnostic tools, and minimally invasive surgical options mean patients today have more effective, less invasive treatments than ever before.
If you have been diagnosed with a lung tumour in Singapore or are experiencing persistent respiratory issues, contact Neumark Lung & Chest Surgery Centre. Our thoracic surgeons provide expert diagnosis, state-of-the-art lung tumour removal and compassionate care tailored to each patient’s needs.

