Metastatic lung cancer represents one of the most challenging frontiers in thoracic oncology, embodying the advanced stage of a disease that continues to be a leading cause of cancer-related mortality worldwide. This complex condition occurs when malignant cells from the primary lung tumour disseminate to distant organs, most commonly the brain, bones, liver and adrenal glands.
The process of metastasis involves a sophisticated cascade of molecular events, enabling cancer cells to detach from the primary tumour, invade surrounding tissues, enter the bloodstream or lymphatic system, and establish new tumours in distant sites.

Diagnosis of metastatic lung cancer necessitates a multidisciplinary approach. Advanced imaging techniques, including high-resolution CT scans, PET-CT, and specialised MRI protocols, have significantly enhanced the ability to detect and characterise metastatic lesions. However, tissue diagnosis remains paramount.
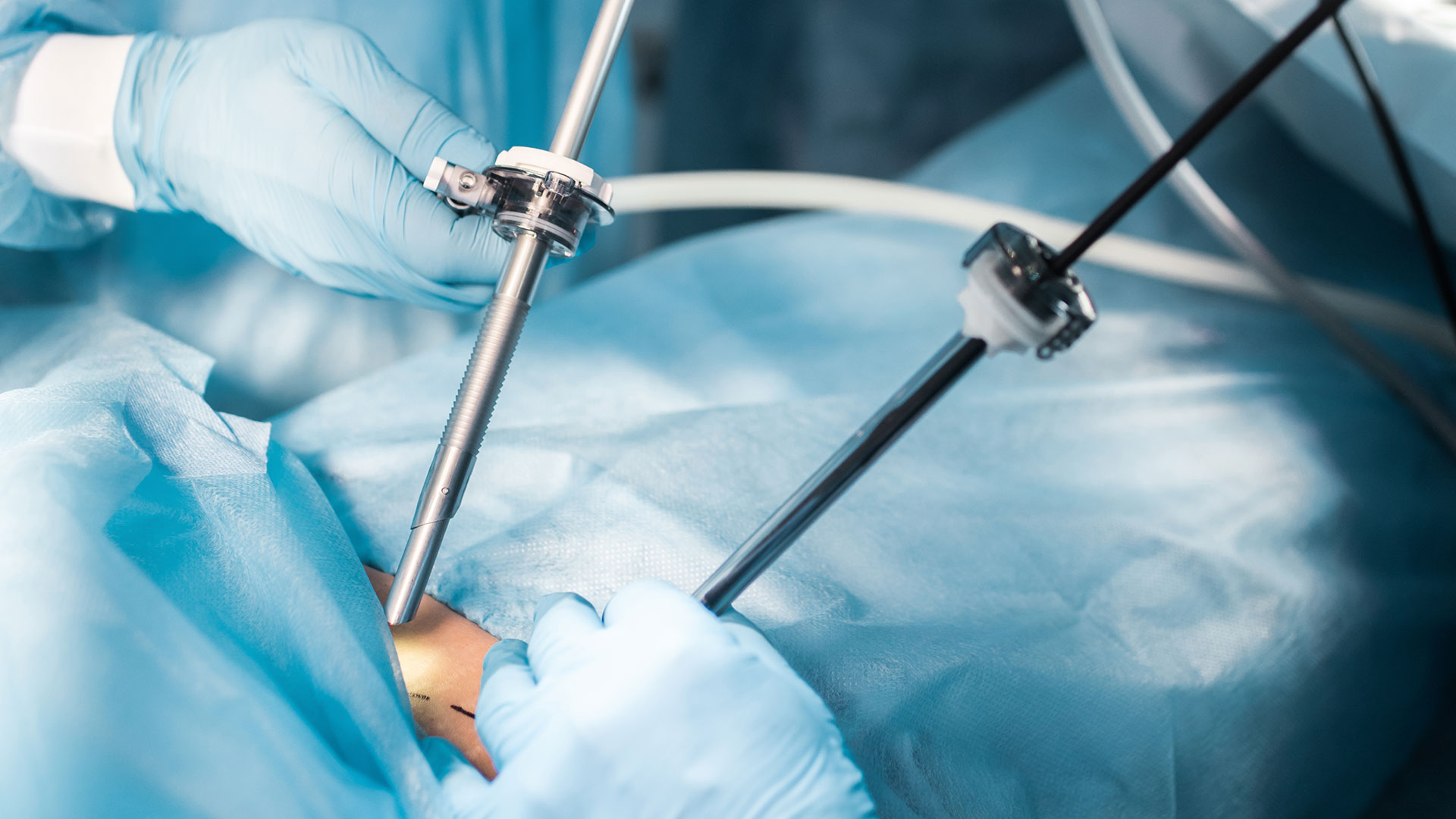
Video-assisted thoracoscopic surgery (VATS) biopsy
Video-assisted thoracoscopic surgery (VATS) has revolutionised tissue acquisition for metastatic lung cancer diagnosis, balancing diagnostic yield and patient comfort. It allows visualisation of the entire pleural cavity and direct sampling, surpassing needle biopsies in effectiveness. VATS is crucial for accessing difficult peripheral lung nodules through 2-3 small incisions. It provides larger tissue samples for comprehensive molecular testing, essential for personalised treatment.
The technique offers faster recovery, less pain, and shorter hospital stays, with many patients discharged within 24-48 hours. While requiring general anaesthesia, VATS’ diagnostic accuracy makes it invaluable for metastatic lung cancer evaluation, enabling rapid treatment initiation when necessary. These samples confirm the diagnosis and provide crucial information about the tumour’s molecular profile, guiding treatment decisions.
Treatment for metastatic lung cancer
The treatment landscape for metastatic lung cancer has undergone a paradigm shift in recent years. While traditionally considered incurable, advances in targeted therapies and immunotherapy have challenged this notion.
Although surgery is not typically the primary treatment modality in Stage IV disease, there are scenarios where surgical intervention can play a role.
In oligometastatic disease cases, where there are a limited number of metastatic lesions, a combination of local therapies (such as surgery or stereotactic radiotherapy) with systemic treatments can lead to long-term disease control in selected patients.
Molecular Testing
The advent of molecular testing has ushered in an era of precision medicine in lung cancer treatment. Mutations in genes such as EGFR, ALK, ROS1, and BRAF, among others, can now be targeted with specific drugs, often yielding remarkable responses. Identifying these mutations has become integral to the diagnostic workup, necessitating sufficient tissue for comprehensive molecular profiling.
Immunotherapy
Immunotherapy, particularly checkpoint inhibitors targeting PD-1/PD-L1, has emerged as a game-changer in the treatment of metastatic lung cancer. These drugs harness the body’s immune system to fight cancer and have shown durable responses in some patients. In certain cases, these treatments can render initially inoperable tumours resectable, opening up new possibilities for multimodality treatment approaches.
Despite these advances, managing metastatic lung cancer remains challenging. Patients often present with complex symptoms that require a nuanced approach. Malignant pleural effusions, a common complication, can cause significant dyspnea. While thoracentesis provides temporary relief, recurrence is common. Indwelling pleural catheters or pleurodesis procedures can offer more durable symptom control and improve quality of life.
The future of metastatic lung cancer management is likely to become increasingly personalised. Liquid biopsies, which analyse circulating tumour DNA in the blood, hold promise for real-time monitoring of disease progression and treatment response. This technology could allow for earlier detection of resistance mechanisms and guide timely treatment modifications.
The future of metastatic lung cancer treatment lies in personalised, multimodality approaches that leverage the strengths of various specialities to offer patients the best possible outcomes and quality of life.