Mediastinal tumours are rare but can affect anyone. Posterior mediastinal tumours, a type of mediastinal tumour, are no different. These masses can affect vital organs and structures essential for various bodily functions, like circulating blood, breathing, and immune responses. While some may be benign tumours that are non-cancerous, others can be malignant cancers that spread and require a swift and effective response from medical professionals.

What Is The Mediastinum
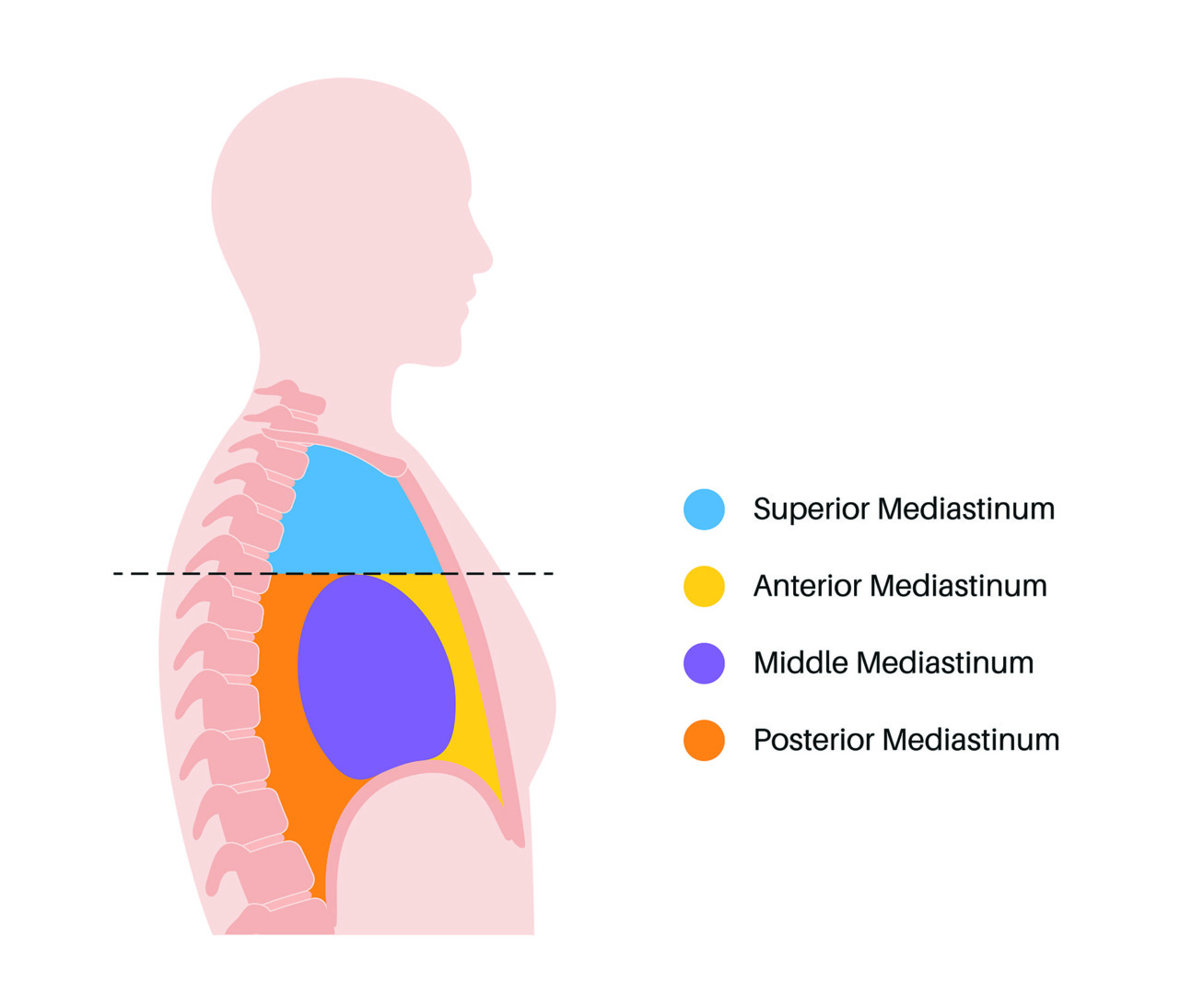
The human chest cavity is home to some of our most important organs, with the mediastinum as the central compartment that divides the lungs. This area contains the heart, major blood vessels, trachea, oesophagus, thymus, lymph nodes and various nerves. When growths develop in this area, they are called mediastinal masses and are classified according to their location in this complex area.
The mediastinum is divided into three main compartments: anterior, middle and posterior. This anatomical understanding is important because the location of a mediastinal mass often gives clues to its nature, risks and treatment approach.
Types of Mediastinal Tumours
Mediastinal tumours are classified into several types, each with its characteristics and treatment.
- Benign tumours, such as thymic cysts and neurogenic tumours, are non-cancerous and do not spread to other body parts. They grow slowly and may not cause any symptoms.
- Malignant tumours like thymoma and thymic carcinoma are cancerous and can invade nearby tissues and metastasise to distant organs.
- Germ cell tumours, lymphomas and neurogenic tumours are common mediastinal tumours. Each has its form of origin. Germ cell tumours come from cells meant to form reproductive cells, lymphomas from lymphatic tissue, and neurogenic tumours from nerve tissue.
Depending on its nature and progression, each type of tumour requires a tailored approach, from surgical removal to chemotherapy and radiation therapy.
What Is A Posterior Mediastinal Mass?
A posterior mediastinal mass is an abnormal growth in the back part of the mediastinum, the area closest to the spine. The posterior mediastinum contains essential structures like the descending aorta, oesophagus, azygos and hemiazygos veins, thoracic duct, sympathetic chain, and portions of the vagus and splanchnic nerves. As a result of this complex anatomy, masses in this area can affect multiple vital systems if left untreated.
Most posterior mediastinal masses arise from neurogenic tissue (tissue related to the nervous system), with about 75% of adult cases being nerve sheath tumours, ganglioneuromas and other neurogenic tumours. Other posterior mediastinal masses can include lymphomas, enteric cysts, meningoceles, extramedullary haematopoiesis (formation of blood cells outside the bone marrow), paravertebral abscesses and descending aortic aneurysms.

Posterior Mediastinal Mass Symptoms
Many posterior mediastinal masses are found incidentally during imaging studies for other conditions. This is because smaller masses do not produce symptoms in the early stages. However, as the mass grows, it can compress or invade surrounding structures and start to cause various symptoms.
The symptoms of a posterior mediastinal mass can vary greatly depending on its size, the structures being compressed or invaded, whether the mass is benign or malignant, the rate of growth, and any associated conditions.
These posterior mediastinal mass symptoms include:
- Pain: Pain is often the first and most common symptom of a posterior mediastinal mass. It can be back pain between the shoulder blades, chest pain that radiates to the shoulders, arms, or neck, pain that worsens when lying down or at night, or discomfort that increases with deep breathing or coughing. The pain from posterior mediastinal masses usually comes from compression of nerve roots or invasion of the chest wall or vertebral bodies.
- Respiratory Symptoms: When a posterior mediastinal mass compresses the airways or lungs, patients may experience shortness of breath (dyspnoea), especially with exertion, persistent cough, wheezing, or stridor (a high-pitched breathing sound), and recurrent respiratory infections.
- Neurological Symptoms: Due to their proximity to the spinal cord and nerve roots, posterior mediastinal masses can cause numbness or tingling in the arms or legs, muscle weakness, difficulty walking, and, in severe cases, paralysis if the spinal cord is compressed.
- Digestive Symptoms: If the mass affects the oesophagus, patients may experience difficulty swallowing (dysphagia), a feeling of food getting stuck, regurgitation, and unintentional weight loss.
- Systemic Symptoms: Some posterior mediastinal masses, especially malignant ones, can cause systemic symptoms like unexplained fever, night sweats, fatigue, weight loss and feeling unwell.
Note that posterior mediastinal mass symptoms can be subtle initially and progress gradually. This subtle presentation can lead to delayed diagnosis, hence the importance of thorough evaluation when persistent chest or back symptoms develop. If you have any of these symptoms, especially persistent back or chest pain, breathing difficulties or neurological symptoms, seek medical attention immediately.
Individuals diagnosed with mediastinal tumours should work closely with their doctor to develop a treatment plan. Regular follow-up appointments and open communication with the doctor are important to manage symptoms, monitor treatment progress, and address any concerns that may arise. This collaborative approach can help individuals navigate their diagnosis and treatment and improve their overall well-being.

Anterior vs Posterior Mediastinal Mass
Anterior mediastinal masses are located in the front portion of the mediastinum in front of the heart and behind the sternum (breastbone). This region contains the thymus gland, lymph nodes and connective tissue. Posterior mediastinal masses develop in the back portion of the mediastinum close to the spine. This area includes the sympathetic nerve chain, descending aorta, oesophagus and thoracic duct.
The types of masses found in each compartment differ: The anterior mediastinal region typically contains thymomas (tumours of the thymus gland), lymphomas, germ cell tumours (teratomas, seminomas), thyroid masses, and parathyroid lesions. In contrast, posterior mediastinal masses are neurogenic tumours (schwannomas, neurofibromas, neuroblastomas), enteric cysts, meningoceles, extramedullary hematopoiesis and paravertebral abscesses.
The age of presentation also differs. Anterior mediastinal masses are more common in adults and often present in the 40-60 age range, though certain types, like lymphomas, can affect younger individuals. Posterior mediastinal masses have a bimodal age distribution. Neuroblastomas and ganglioneuroblastomas affect children, while nerve sheath tumours (schwannomas and neurofibromas) are more common in adults.
The symptoms of anterior versus posterior mediastinal masses differ due to the structures they affect. Anterior mediastinal masses cause respiratory symptoms (cough, shortness of breath), superior vena cava syndrome (facial swelling, distended neck veins) and systemic symptoms like fever and weight loss. They may also be associated with paraneoplastic syndromes like myasthenia gravis with thymomas.
Posterior mediastinal masses cause back pain, neurological symptoms due to nerve or spinal cord compression and digestive symptoms if the oesophagus is involved. They are less likely to present with respiratory symptoms unless they grow large enough to compress lung tissue.

Related Mediastinal Conditions
Diagnosing a Posterior Mediastinal Mass
Diagnosing a posterior mediastinal mass necessitates a systematic approach that begins with a thorough clinical evaluation and progresses through various imaging studies and, if necessary, tissue biopsy.
The diagnostic journey begins with:
- Comprehensive medical history: Assessment of symptoms, duration, progression and risk factors
- Physical examination: Evaluation of vital signs, respiratory examination, neurological assessment and palpation for any associated lymphadenopathy
- Review of systems: Checking for associated symptoms that may provide clues about the nature of the mass. Imaging is key in detecting and characterising posterior mediastinal masses:
- Chest X-ray: Often the first imaging study to detect an abnormality in the chest, but provides limited information about the mass characteristics or exact location.
- Computed Tomography (CT) Scan: The gold standard for initial evaluation of mediastinal masses, CT scans provide detailed information about the exact location and extent of the mass, its relationship to surrounding structures, its density characteristics (solid, cystic, fatty components), evidence of invasion into adjacent structures, and the presence of calcifications or enhancement patterns.
- Magnetic Resonance Imaging (MRI): Particularly useful for posterior mediastinal masses due to its superior soft tissue contrast, ability to assess spinal involvement, better characterisation of neurogenic tumours and ability to distinguish between vascular structures and solid masses without contrast.
- Positron Emission Tomography (PET) Scan: Useful if malignancy is suspected, as it can assess metabolic activity of the mass, detect distant metastases, guide biopsy by identifying the most active areas of the tumour and aid in treatment planning and response assessment.

Biopsy of Posterior Mediastinal Mass
In many cases, a definitive diagnosis requires tissue sampling through biopsy. The approach to biopsy of posterior mediastinal mass depends on the location, size and suspected nature of the lesion:
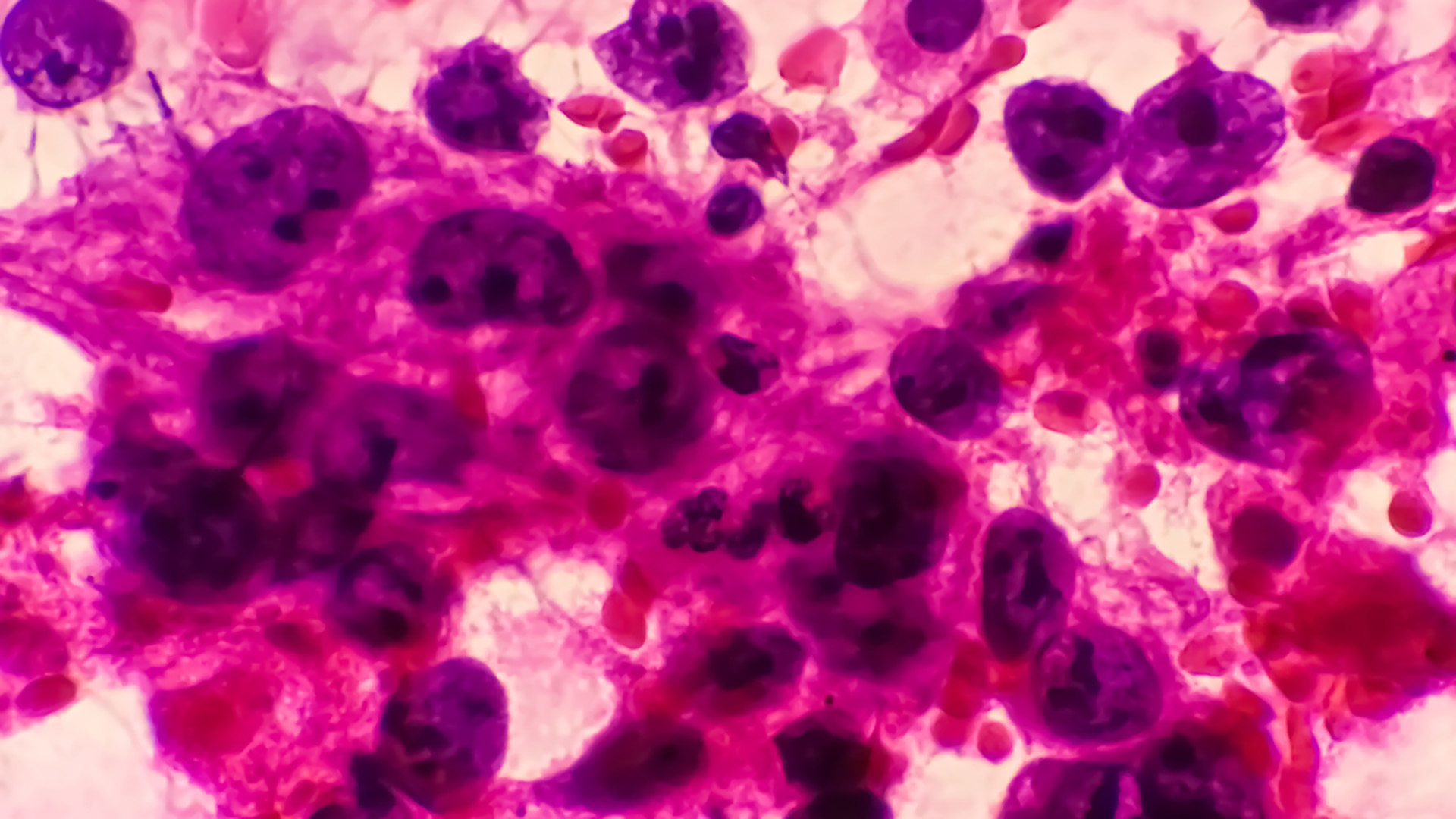
- CT-guided Needle Biopsy: This is the most common initial approach that is minimally invasive, can be done under local anaesthesia, provides tissue for cytological and limited histological examination and carries risk of bleeding, pneumothorax (collapsed lung) and false negative results due to sampling error.
- Endobronchial Ultrasound (EBUS)-guided Biopsy: This type of biopsy is used for masses adjacent to the airways, and uses an ultrasound probe on a bronchoscope to visualise and sample the mass, minimises the risk of pneumothorax and provides real-time visualisation during sampling.
- Endoscopic Ultrasound (EUS)-guided Biopsy: This biopsy is particularly useful for posterior mediastinal masses adjacent to the oesophagus, performed through an endoscope placed in the oesophagus, allows access to areas difficult to reach with CT-guided approaches and reduces the risk of traversing vital structures.
- Surgical Biopsy: This is required when less invasive methods are inconclusive or contraindicated, including video-assisted thoracoscopic surgery (VATS) for tissue sampling, mediastinoscopy for certain locations and occasionally open biopsy via thoracotomy for difficult-to-reach areas.
A biopsy of a posterior mediastinal mass is extremely important to determine if the tumour is benign or malignant, identify the specific tumour type and subtype, perform immunohistochemical studies to confirm diagnosis, perform molecular testing for targeted therapies if applicable, and guide treatment decisions.
In some cases, particularly with neurogenic tumours that have classic imaging appearances and are candidates for complete surgical resection, biopsy might be deferred in favour of proceeding directly to definitive surgical removal.

Posterior Mediastinal Mass Treatment
Treating posterior mediastinal masses requires a tailored approach based on the specific diagnosis, extent of the mass, patient’s symptoms and overall health status. Neumark Lung & Chest Surgery Centre uses a holistic, multidisciplinary approach to deliver the best care for each patient.
Several factors influence the posterior mediastinal mass treatment strategy, including the benign vs. malignant nature of the mass, its size and exact location, the involvement of surrounding structures, the patient’s symptoms and functional status, and overall health and comorbidities.

Surgical Management of Posterior Mediastinal Tumours (VATS & RATS)
Surgery is the mainstay of treatment for most posterior mediastinal masses, particularly neurogenic tumours. While less commonly used today for straightforward cases, an open thoracotomy may be necessary for large tumours, masses with significant invasion of surrounding structures, cases where minimally invasive approaches are contraindicated, and situations requiring complex reconstruction.
However, Neumark Lung & Chest Surgery Centre usually recommends minimally invasive surgical approaches, such as Video-Assisted Thoracic Surgery (VATS) and Robotic-Assisted Thoracic Surgery (RATS).
VATS has changed the surgical management of posterior mediastinal masses by requiring only small incisions (1-3 cm), excellent visualisation through high-definition cameras, less postoperative pain and recovery time, less blood loss and tissue trauma, earlier return to normal activities, and fewer wound complications. This involves inserting a video camera and special instruments through small incisions between the ribs, allowing the surgeon to visualise and remove the mass without spreading the ribs.
As a new advancement in posterior mediastinal mass treatment, RATS has several advantages over traditional surgery, including 3D visualisation, greater precision through instruments with 7 degrees of freedom, better manoeuvrability in tight spaces near the spine, better ergonomics for the surgeon (potentially more precise dissection), reduced hand tremor through computer filtering, and the ability to perform complex procedures through minimally invasive approaches.
Our surgeons are trained in robotic techniques to remove masses that would otherwise require open surgery due to their location or relationship to vital structures.

Challenges in Managing Posterior Mediastinal Masses
Despite advances in diagnosis and treatment, posterior mediastinal masses present challenges:
- Anatomical Complexity: The posterior mediastinum contains vital structures in close proximity, including the descending aorta, oesophagus, thoracic vertebrae, spinal cord and major nerves, including the vagus and sympathetic chain. This anatomical complexity requires surgical expertise and precision to avoid complications.
- Malignant Transformation: Some benign neurogenic tumours can become malignant if left untreated, so even asymptomatic lesions may need to be managed.
- Multidisciplinary Care: Complex cases often require thoracic surgeons, neurosurgeons, medical oncologists, radiation oncologists, radiologists, pathologists, pain specialists and physiotherapists. Neumark Lung & Chest Surgery Centre offers a multidisciplinary approach that ensures tailored care for each patient.

When to See A Thoracic Surgeon
Early detection and treatment of posterior mediastinal masses gives the best chance of good outcomes and minimal complications. Call Neumark Lung & Chest Surgery Centre now at +65 6908 2145 or WhatsApp us at +65 9726 2485 to book an appointment with one of our thoracic surgeons—your health matters.

