In cases where thymomas are malignant, thymectomy is also performed to prevent the spread of cancer. With advancements in surgical techniques, particularly the use of minimally invasive methods such as the da Vinci Robotic Surgery system, thymectomies have become safer, with reduced recovery times and complications.
Thymomas and Myasthenia Gravis
Myasthenia gravis, characterised by its signature symptoms of muscle weakness and fatigue, poses a significant clinical challenge, particularly when compounded by thymoma tumours in the thymus gland. These tumours necessitate a surgical approach that is both effective and considerate of the patients’ fragile condition.
Thymectomy indications in myasthenia gravis patients, which occur in about 15% of cases, can complicate the clinical approach to the procedure.
The surgical removal of the thymus gland, known as thymectomy, is commonly recommended for individuals with myasthenia gravis who also have a thymoma. The rationale behind this recommendation lies in both the prevention of potential malignancy and the management of myasthenia gravis symptoms. Thymomas, or tumours of the thymus gland, carry a risk of turning cancerous, and their removal is a preventative measure against such malignant transformation.

The novel technology da Vinci Robotic surgical system represents a shift in the surgical management of thymoma in myasthenia gravis patients. The system offers precision and control previously unattainable in conventional surgical removal of the thymus gland to improve operative outcomes and potentially reduce perioperative morbidity.
Importance of the Thymus Gland
The thymus, located behind the sternum, plays a key role in early immune system development, particularly in the maturation and education of T-lymphocytes. This process is vital for distinguishing between foreign invaders and the body’s own cells. As people age, the thymus typically undergoes involution, a natural process where it reduces in size and activity.
The pathophysiology of myasthenia gravis involves complex interactions within the immune system, and the thymus is one of the key organs implicated in these processes. Theories about intrinsic thymic factors that might lead to the generation of autoreactive cells and possible genetic predispositions to such autoimmune responses are being explored.
Current research supports the hypothesis that the thymus in myasthenia gravis patients may be involved in the abnormal production of T-lymphocytes. These cells could contribute to the autoimmune response against acetylcholine receptors, resulting in the characteristic muscle weakness and fatigue from the disease. However, the exact mechanisms of how the thymus contributes to or exacerbates myasthenia gravis are yet to be fully understood and remain an active area of clinical research.
Our Immune Systems Misguided Offensive
Thymomas, tumours originating from the thymus gland, are intricately related to immune processes. The thymus, a crucial site for T-cell maturation, is pivotal in establishing immune tolerance. However, the development of thymomas can disrupt this function, leading to abnormal T-cell activities and potentially giving rise to autoimmune disorders, with myasthenia gravis being the most common.
In myasthenia gravis, the immune system targets acetylcholine receptors at the nerve-muscle junctions, impairing signal transmission and resulting in characteristic muscle weakness. Thymomas can exacerbate this autoimmune response by altering the typical immune-modulating functions of the thymus. Additionally, thymomas are associated with paraneoplastic syndromes, where either the tumour itself or the immune response it triggers can lead to conditions like myasthenia gravis.
The surgical removal of the thymus, or ‘robotic thymectomy’, offers dual benefits in the context of myasthenia gravis with concurrent thymomas. Firstly, it addresses the immediate concern of the tumour, potentially preventing its malignant transformation. Secondly, thymectomy has been observed to alleviate the symptoms of myasthenia gravis in many patients. While the exact mechanism of this symptomatic relief remains an area of ongoing research, it is hypothesised that removing the thymus, including any aberrant immune cells within, may reduce the autoimmune activity against acetylcholine receptors.
Clinical studies evaluating post-thymectomy outcomes have proposed several theories to explain the observed symptom relief in myasthenia gravis. One theory suggests that thymectomy alters the immune response, potentially decreasing the autoimmune attack on nerve-muscle junctions. Another line of thought is that the thymus in myasthenia gravis patients may harbour abnormal immune cells contributing to the disease, and their removal could mitigate the autoimmune response. Further research also indicates that thymectomy might decrease the production of autoantibodies targeting acetylcholine receptors.
However, it is crucial to acknowledge that thymectomy does not uniformly improve symptoms in all myasthenia gravis patients, and the extent of improvement varies.
Factors influencing the decision and outcome of thymectomy include the patient’s age, the severity of myasthenia gravis symptoms, the presence of a thymoma, and the patient’s overall health status. Therefore, the decision to proceed with thymectomy must be made on a case-by-case basis, considering the individual patient’s clinical profile. This decision-making process underscores the complexity of myasthenia gravis and the multifaceted nature of its management, an area that continues to evolve with ongoing medical research.
da Vinci Robotic Surgical Revolution
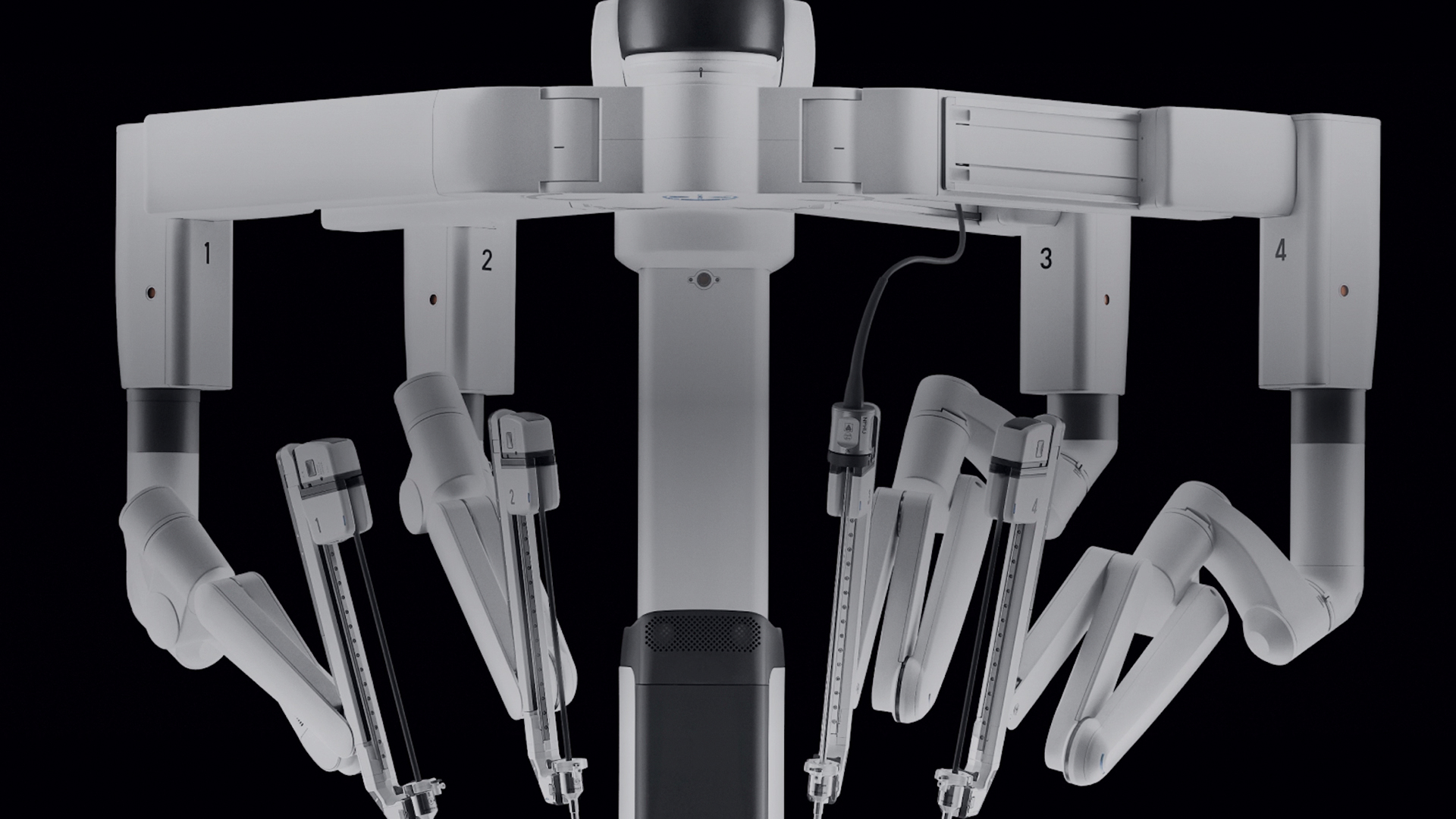
The da Vinci Surgical System represents a significant advancement in minimally invasive surgery and has particular applications in the resection of the thymus, especially relevant for patients with myasthenia gravis. The system offers several key benefits of thymectomy in myasthenia gravis over traditional open surgeries, which can lead to improved operative outcomes:
- Targeted Removal with Minimal Impact
Myasthenia gravis often results in muscle weakness, making patients more vulnerable to the stresses of surgery. The da Vinci system’s precision is crucial and allows for the targeted removal of the thymus (and thymoma, if present) with minimal disturbance to surrounding tissues. This precision is vital in reducing the overall physiological stress of surgery, which is an important consideration for patients with myasthenia gravis.
- Reduced Risk of Myasthenic Crisis
Patients with myasthenia gravis are at risk of a myasthenic crisis, a severe exacerbation of muscle weakness that can be life-threatening and is often triggered by stress on the body. The less invasive nature of robotic-assisted surgery potentially reduces this risk compared to more invasive traditional surgical approaches.
- Better Management of Complications
The enhanced visualisation and precision of the da Vinci system can be particularly beneficial in managing and avoiding intraoperative complications, which is significant for myasthenia gravis patients. Careful dissection around the thymus is crucial to avoid damage to the nearby structures, such as the phrenic and vagus nerves, which can have serious implications in myasthenia gravis.
- Customised Surgical Approach
Myasthenia gravis patients can have varied presentations and severities of the disease, which may necessitate a tailored surgical approach. The da Vinci system offers the flexibility to adapt the surgical technique to each patient’s specific needs and anatomical considerations. This adaptability is a significant advantage in achieving the best possible outcomes for individuals with myasthenia gravis.
- Potential for Symptom Improvement Post-Surgery
The precise removal of the thymus, especially of thymomas, is likely to improve the symptoms of myasthenia gravis. The da Vinci system’s ability to perform this task with greater accuracy and less collateral damage may enhance the likelihood of symptom improvement post-surgery.
- Facilitating Early Mobilisation and Rehabilitation
The minimally invasive nature of the da Vinci-assisted thymectomy typically allows for a quicker thymectomy post-op care. This aspect is particularly beneficial for myasthenia gravis patients, as it facilitates earlier mobilisation and rehabilitation, which are crucial in managing and improving their symptoms.
- Cosmetic Advantage of Reduced Scarring
Beyond these health benefits, from an aesthetic perspective, smaller incisions lead to reduced scarring. This has cosmetic advantages and lessens the chance of restrictive adhesions, which can sometimes cause complications post-surgery.
Using the da Vinci Surgical System for thymectomy in myasthenia gravis patients brings specific advantages that align with this condition’s unique challenges and needs. Its precision, minimal invasiveness, and adaptability to individual patient needs make it a valuable tool in managing myasthenia gravis, especially in cases complicated by the presence of a thymoma.
Leading the Treatment of Thymoma
Neumark Lung and Chest Surgery Centre specialises in thoracic care to provide optimal patient outcomes as we strive towards a healthier future. If you are navigating a recent diagnosis of thymoma, particularly in conjunction with myasthenia gravis, we encourage you to arrange a consultation with Dr Harish Mithiran.
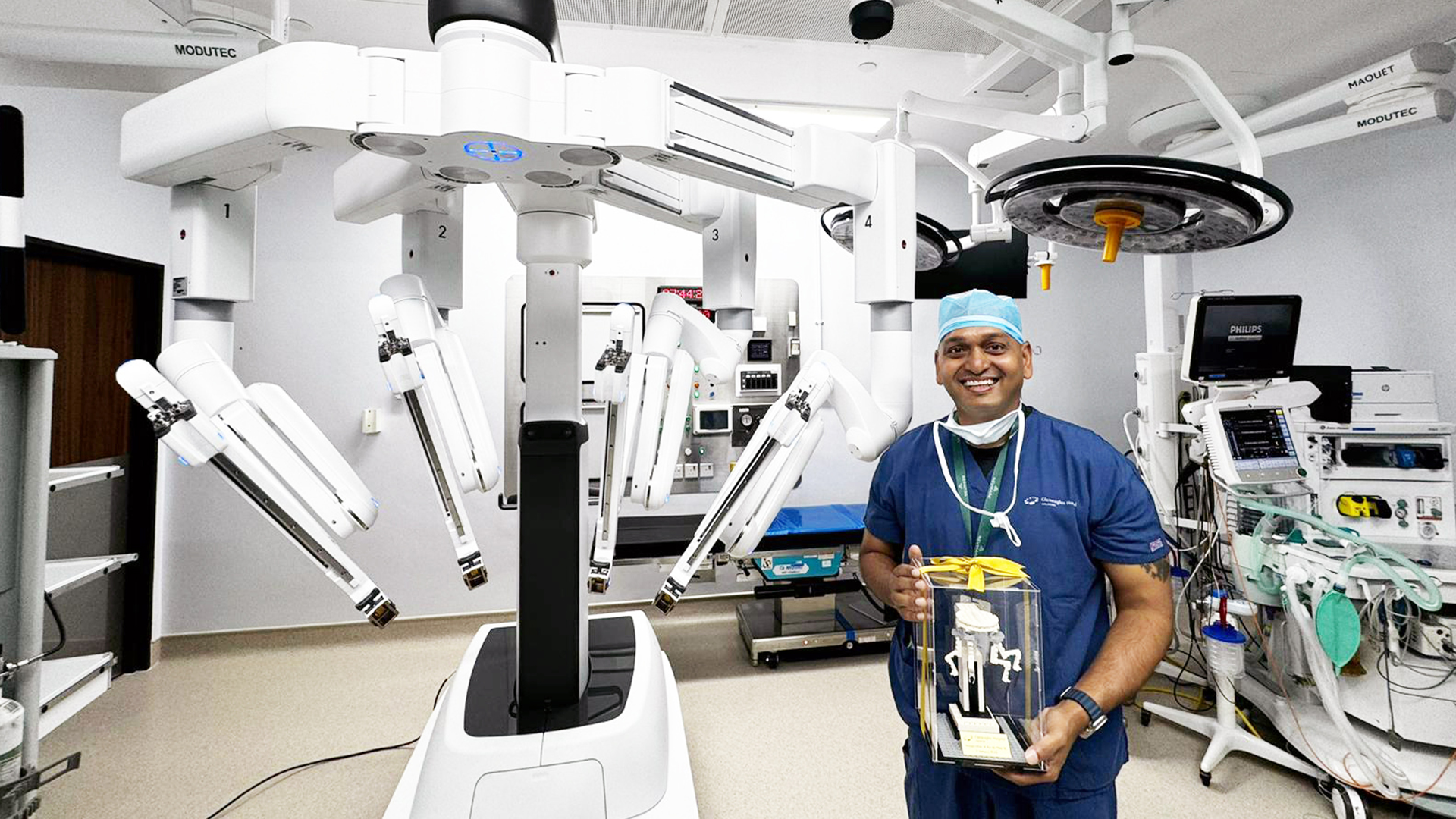
As the director of our centre and a seasoned thoracic surgeon at Gleneagles Hospital, Dr Mithiran brings a wealth of expertise and a patient-centred approach to address your unique medical needs.

