A pulmonary nodule is a small round opacity less than 30mm in diameter in the pulmonary interstitium — the space between the air sacs and the small blood vessels surrounding them where the exchange of gases happens. Pulmonary nodules are common and often an incidental finding during a screening for a different chest issue. They are found in 20% – 50% of healthy adult lung cancer screening populations.
Just because a nodule is present doesn’t mean it’s malignant, but it’s an important sign that needs to be evaluated by a lung specialist. Nodules under 8mm rarely need to be concerned about and are often benign findings. Nodules 8-30mm in size need to be looked into further, and anything above 30mm is usually of high concern. However, size alone doesn’t determine malignancy risk. These small lung issues can come from many underlying conditions, from benign inflammatory processes to early-stage malignancies.

Detection and Diagnostic Pathway
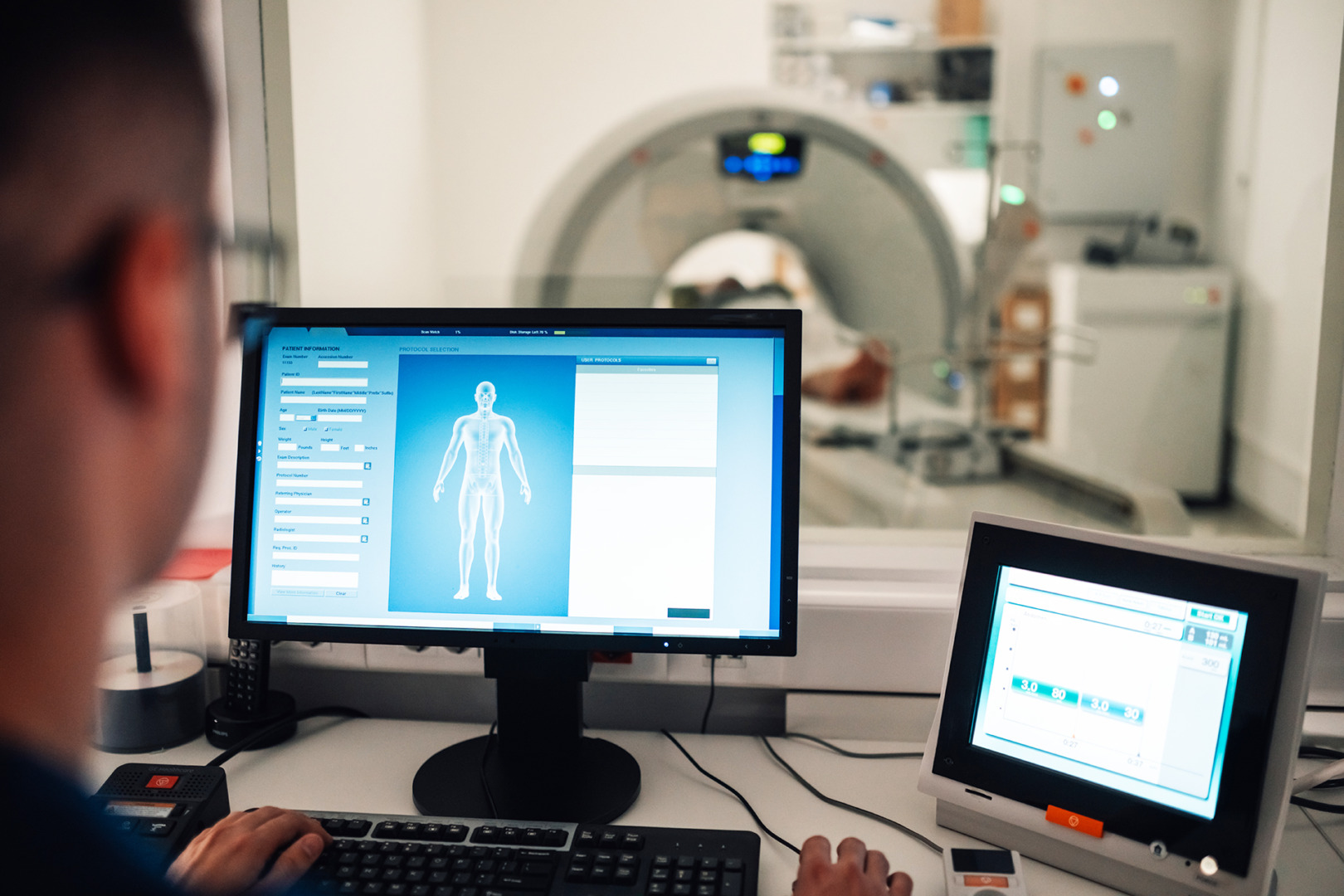
Modern imaging has made it possible to detect and analyse pulmonary nodules with great precision. CT chest scans, the gold standard for detecting pulmonary nodules, provide radiologists with a 3D view of them to assess their size, shape, and characteristics.
Clinicians use a risk stratification approach when evaluating pulmonary nodules. The nodule size, patient age, smoking history and other medical comorbidities are important in determining the diagnostic pathway. Not all nodules are cause for alarm. Many are incidental findings that require monitoring rather than intervention.
Lung Cancer Screening and Pulmonary Nodules
Regular check-ups and screening are the best way to catch lung cancer early, especially for high-risk individuals like smokers or those with a family history of the disease. Lung cancer screenings are a tool for the early detection and treatment of lung cancer. Lung cancer mortality is decreasing with annual low-dose CT screening in high-risk individuals. Early detection is key. The 5-year survival rate is around 70% for non-small cell lung cancer when caught in Stages I and II. This is compared to 21% for all stages combined and 4% for Stage IV.
Early detection, advanced diagnostics, and minimally invasive surgery have transformed what was once a worrying diagnosis into a manageable condition. Understanding pulmonary nodules isn’t just about peace of mind. It’s about empowering patients with knowledge of their respiratory health. By staying proactive and seeking expert evaluation, patients can improve their prognosis and take control of their lung health.

Risk Factors and Epidemiology
Specific demographic and lifestyle factors, as well as patient risk factors, greatly influence pulmonary nodule development. Patients with extensive smoking history, occupational exposure to environmental carcinogens, or a family history of lung disease are at higher risk. Advanced age correlates with higher nodule prevalence, so regular medical screening is important for vulnerable populations. Emerging research suggests that air pollution, chronic respiratory diseases and genetic predisposition may contribute to developing pulmonary nodules.
The differential diagnosis for pulmonary nodules includes malignancy and inflammatory, infectious, congenital, and vascular pathologies. Most (> 95%) incidental pulmonary nodules are benign, even in lung cancer screening populations. However, some pulmonary nodules can be signs of early small cell lung cancer. A thorough evaluation, including clinical assessment, radiological imaging, and sometimes a biopsy, is needed to determine the nature of a pulmonary nodule.
Radiological Imaging and Nodule Characteristics
Radiological imaging is a key component in diagnosing and managing pulmonary nodules. Chest CT with thin (≤ 1mm) sections is more accurate than chest X-rays in detecting nodules. PET is sometimes used to evaluate larger, higher-risk pulmonary nodules. Low-dose CT (LDCT) is a common surveillance imaging tool; in this case, contrast is not usually required.
Pulmonary nodules can be described by size, morphology and/or distribution. The size of pulmonary nodules can vary from a few millimeters to several centimeters in diameter. The morphology of pulmonary nodules can be solid, part-solid, or non-solid. Small pulmonary nodules (< 6mm) are often benign, and larger nodules (> 20mm) are more likely to be malignant. Distribution of pulmonary nodules can be solitary, multiple or diffuse.

Advanced Diagnostic Techniques
PET scans can differentiate between benign and potentially malignant nodules by measuring metabolic activity. Minimally invasive techniques like CT-guided needle biopsies provide definitive cellular-level information without requiring extensive surgery. For small nodules with concerning features, bronchoscopy with endobronchial ultrasound (EBUS) allows real-time imaging and guided biopsy collection, improving diagnostic accuracy with minimal patient discomfort. Evaluating a solitary pulmonary nodule is key in identifying lung cancer, guided by clinical guidelines and studies.
Surgical Intervention with RATS and U-VATS
Modern thoracic surgery has made the patient experience better through minimally invasive techniques for the surgical evaluation of pulmonary nodes.
Robotic-Assisted Thoracic Surgery (RATS) is the pinnacle of surgical innovation, offering unparalleled precision and a shorter recovery time than most other surgical methods. Surgeons can use robotic technology to manipulate instruments with unbelievable dexterity, allowing complex lung procedures through tiny incisions. This reduces surgical trauma and enhances patient safety and long-term outcomes.
Uniportal Video-Assisted Thoracoscopic Surgery (U-VATS) is another innovative option that uses a single small incision, reducing surgical trauma while maintaining diagnostic and therapeutic capabilities. Patients have shorter hospital stays, minimal scarring, and faster recovery. U-VATS also allows minimally invasive wedge resection to remove nodules, preserving as much lung tissue as possible and ensuring thorough pathological analysis.

Management and Surveillance
There is no single approach to the management of lung nodules. Some nodules require immediate intervention, while others require a long-term surveillance approach. Radiological follow-up protocols are designed, often involving sequential CT scans to monitor changes over time. For low-risk nodules, serial imaging at set intervals will detect any suspicious growth early. Biopsy or surgical excision may be needed for higher risk cases to rule out malignancy.
Interdisciplinary collaboration is key. Pulmonologists, radiologists, oncologists, and thoracic surgeons collaborate to synthesise complex clinical information and formulate individualised patient management plans.

Expert Care at Neumark Lung & Chest Surgery Centre
At Neumark Lung & Chest Surgery Centre, we specialise in diagnosing and treating pulmonary nodules with a full range of imaging tests, minimally invasive procedures and expert surgical interventions. Whether you need advanced diagnostic evaluation, precise surgical removal or surveillance, our team is committed to patient-centred, world-class care.
Concerned about pulmonary nodules or want an expert evaluation? Contact Neumark Lung & Chest Surgery Centre today. Our team of experts is dedicated to comprehensive, compassionate care for your individual needs.

