Video-Assisted Thoracoscopic Surgery (VATS), also known as ‘keyhole surgery’, is a surgical procedure for the chest and lungs that uses a tiny video camera and surgical instruments inserted through small incisions. Compared to traditional open surgery and open-chest surgery, VATS tends to result in less postoperative pain, a shorter hospital stay, and a faster recovery. Still, the right approach for each patient will depend on a host of factors, including diagnosis, lung function, and the surgeon’s goals.
At Neumark Lung & Chest Surgery Centre in Singapore, decisions to opt for Video Assisted Thoracoscopic Surgery are made after careful assessment by specialists and multidisciplinary teams, led by senior consultant thoracic surgeon Dr Harish Mithiran at Gleneagles and Mount Alvernia hospitals.

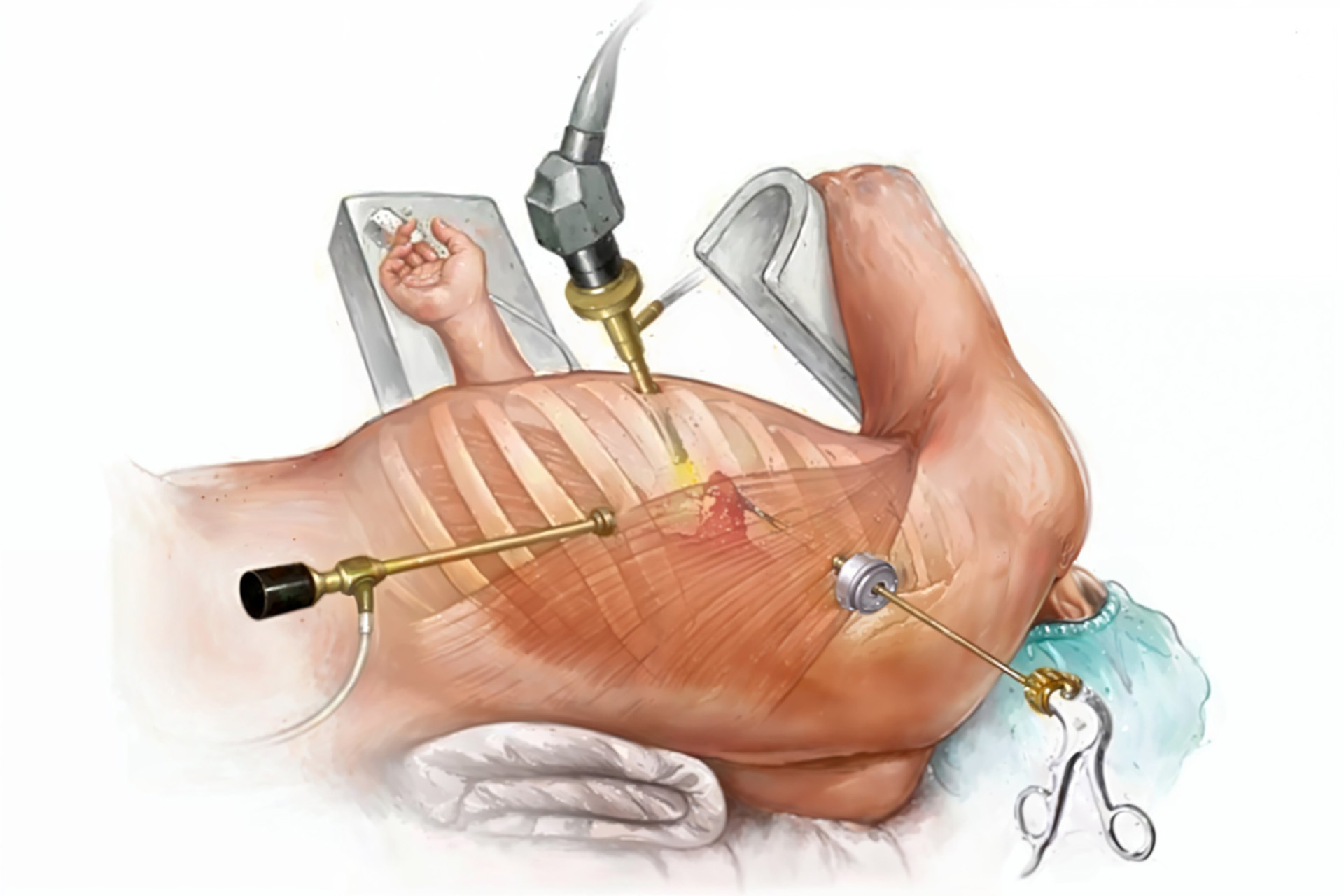
VATS involves making a couple of small incisions between the ribs to insert a tiny camera called a thoracoscope (a tiny video camera) that lets the surgeon see what’s going on inside the chest cavity on a video monitor. The surgeon then uses special surgical instruments to perform actions like removing lung nodules, taking biopsies, treating lung cancer, treating problems like collapsed lung or performing cancer surgery, all through small incisions.
Video-assisted thoracic procedures are not just an easy alternative to the open chest approach of surgery. Despite reducing chest wall damage, Video-Assisted Thoracoscopic Surgery is complex, requiring expertise to perform delicate internal operations, such as cancer removal, safely.
Some of the common conditions treated with VATS procedures include:
Your surgeon should be able to explain whether VATS is recommended for diagnosis, treatment, or both.

Thoracic surgeons carefully consider the trade-offs of Video-Assisted Thoracoscopic Surgery versus open approaches. They must balance the advantage of a smaller incision against the need for clear visualisation and a safe procedure. Key considerations include:
Video-assisted thoracic care and assisted thoracoscopic procedures aren’t one-size-fits-all. There are several techniques thoracic surgeons use, and the choice depends on the individual patient and the operation. For example:
While the technique used is necessary, the surgeon’s experience and judgment are key. The aim is to achieve the safest possible and optimal outcome, with a tailored recovery plan for each patient.
VATS can offer a range of benefits, including reduced postoperative pain, faster mobilisation, a shorter hospital stay, a quicker recovery time, and an earlier return to normal activities. For some patients with early-stage lung cancer, the outcomes are comparable to traditional open surgery, but only if they get the proper care and follow-up.
Patients also benefit from reduced infection risk, as the technique minimises tissue trauma and exposure during surgery. Aesthetically, VATS leaves minimal scarring compared to traditional open surgery, as it requires only small incisions, which can have a serious psychological benefit for many patients.
VATS is an equally effective alternative to conventional surgery for patients who qualify, with the added advantage of enabling a quicker return to daily activities. However, it’s worth keeping your expectations in check. Recovery time will vary. Your baseline overall health will also play a significant role in your post-surgery recovery. Healthcare providers will guide your healthy recovery.

Determining whether a patient qualifies for Video-Assisted Thoracic Surgery (VATS) involves carefully evaluating multiple factors, including their specific condition, overall health status, and surgical history. Many patients with early-stage lung cancer, pleural effusion, or other localised thoracic conditions make excellent candidates for this minimally invasive approach.
However, VATS may only be suitable for some. Patients with extensive previous chest surgeries or significant scarring might require traditional surgical methods instead, as scar tissue can affect the feasibility. Given these considerations, a thorough consultation with an experienced thoracic surgeon becomes crucial in determining the most appropriate surgical approach for each case.
Like any surgical procedure, VATS carries risks and possible complications. It involves operating on delicate thoracic structures and surrounding tissues, which increases the risk of bleeding, infection, pneumonia, prolonged air leaks, or wound complications. Wound care is essential to prevent infection. Some patients may have altered sensations around the small incisions, and in rare cases, there may be a risk of more serious complications. Blood clots are also a possible complication, so measures to prevent them are taken.
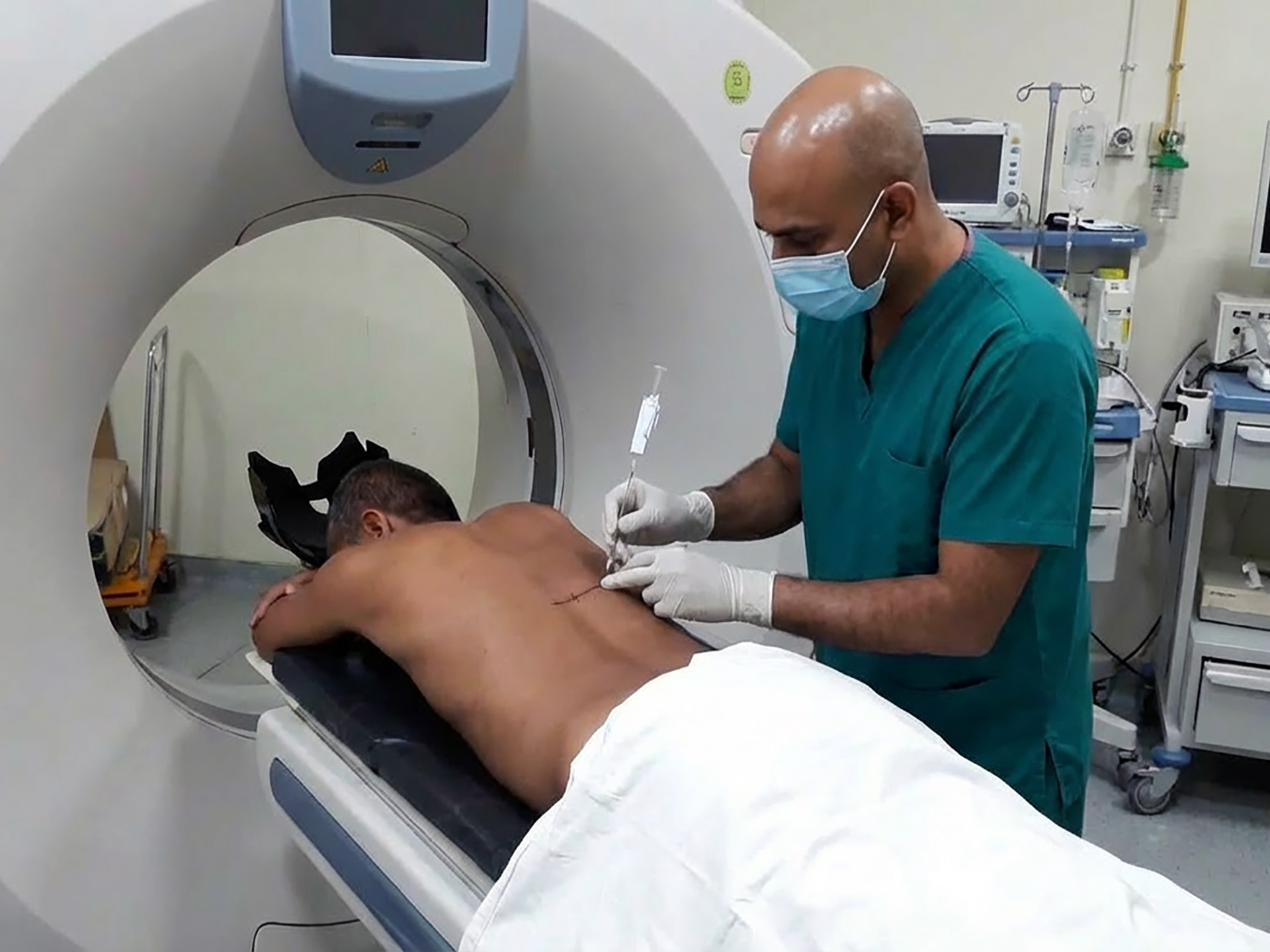
The pre-operative process confirms the diagnosis, aligns the surgical plan, and ensures the safety and competence to proceed with the operation, likely involving:
Here in Singapore, thoracic surgeons often refer GPs for polyclinic workups, screening, or specialist referrals after a CT scan. That way, people can get the care they need quickly and smoothly, without undergoing unnecessary tests.

Recovery from VATS can be challenging, but with a medical team’s support, you should be fine. The first 24-48 hours will focus on pain control, deep breathing, and movement. You can think of recovery as split into three parts: hospital, home and follow-ups.
In Hospital
Chest tubes may be needed temporarily. The staff will monitor lung expansion, oxygen saturation, and pain, and encourage exercises to minimise any complications.
At Home
Most patients are discharged within days, depending on the procedure complexity, chest tube duration, and recovery speed. Fatigue is common during recovery. Minor procedures allow a return to normal in 1-2 weeks. Major operations may take a few weeks. Work clearance depends on pain, job type, and the surgeon’s advice.
Follow-Up and Results
The pathology reports will dictate what happens next. For cancer surgical procedures, the lymph node status and the type of tumour will help determine the staging and whether you need any further treatment.
Video-Assisted Thoracoscopic Surgery works well for selected early-stage lung cancer, with techniques such as VATS lobectomy and lymph node removal for staging. When used correctly, video-assisted thoracoscopic surgery can produce results that are comparable to open chest surgery.
VATS isn’t suitable for all cases. Traditional open surgery or alternatives are better for very central/locally advanced tumours or significant chest wall scarring. Other treatments, such as conventional open procedures, stereotactic radiotherapy for small cancers, or targeted procedures, might be a better fit if the disease is extensive, there are dense adhesions, or complex tumours that require major reconstruction.
Effective lung cancer treatment requires the right team working together. That means having a thorough consultation to figure out the best approach for your specific situation.

Select a thoracic care team with experience, strong communication, and comprehensive support from diagnosis to recovery. Effective care requires a centre that coordinates all aspects, including imaging, biopsies, oncology, and follow-ups, going beyond just the surgery, VATS or otherwise.
Ask about decision-making, complication handling, expected follow-ups and pain relief. While technology is crucial, surgical judgment and experience are paramount.
Neumark Lung & Chest Surgery Centre, run by Dr Harish Mithiran, is focused on minimally invasive thoracic procedures (VATS, U-VATS, robotic approaches). We offer multidisciplinary care for complex thoracic conditions, including lung cancer, pleural disease, and mediastinal tumours, at both Gleneagles and Mount Alvernia hospitals in Singapore. We focus on making your journey as smooth as possible and achieving optimal outcomes with fewer complications. Make an appointment today to learn more about VATS and how Neumark can support you.
Not always. VATS can reduce chest wall trauma, but open surgery may be safer or more effective in complex cases. The best approach is the one that achieves the surgical goal safely.
Many patients report less pain than with open surgery, but pain varies by procedure and individual factors. Modern pain control and early mobilisation make a meaningful difference for both short-term and long-term recovery.
This depends. Many minor diagnostic procedures may allow a return within one to two weeks, while larger resections may take several weeks. Your surgeon will advise based on your job demands and recovery process.
Sometimes, but it depends on the purpose. VATS may be used for diagnosis, staging, symptom relief, or selected treatment steps, but advanced cancer often requires systemic therapy and multidisciplinary planning.
DISCLAIMER: The information provided on this website is for general informational purposes only and is not intended as a substitute for professional medical advice, diagnosis, or treatment. The use of this website does not create a doctor-patient relationship and no medical advice should be inferred or assumed. It is the user’s sole responsibility to seek the advice of their healthcare professionals for any medical concerns they may have and the user should not disregard, or delay, prompt medical advice for any such condition.
Read our latest insights on lung diseases and chest conditions, including prevention tactics, treatments, and more.
Gleneagles Medical Centre
6 Napier Road
#02-09 Gleneagles Medical Centre
Singapore 258499
Mount Alvernia Hospital
820 Thomson Road
#06-07 Medical Centre A
Singapore 574623