Stage 2 lung cancer treatment usually centres on surgery to remove the tumour, supported by chemotherapy, radiotherapy and/or newer drug therapies. At Neumark Lung & Chest Surgery Centre in Singapore, lung cancer treatment is managed by a multidisciplinary team led by senior consultant thoracic surgeon Dr Harish Mithiran, based in Gleneagles and Mount Alvernia hospitals. With careful staging and minimally invasive techniques, many patients can achieve long-term control and a good quality of life under Neumark’s care.
About Lung Cancer
Lung cancer starts when abnormal cells grow uncontrollably in lung tissue, forming a tumour that can interfere with normal breathing and spread to other parts of the body. It is one of the most common types of cancer worldwide and remains a leading cause of cancer death in Singapore.
There are two main types of lung cancer:
- Non-small cell lung cancer (NSCLC), which accounts for about 85% of lung cancer cases, includes subtypes such as squamous cell carcinoma, adenocarcinoma and large cell carcinoma.
- Small cell lung cancer (SCLC), which makes up the remaining 15%, tends to grow and spread more quickly.
Early detection through lung cancer screening can make a significant difference, as treating lung cancer at an early stage offers the best chance for successful outcomes.
What Is Stage 2 Lung Cancer?
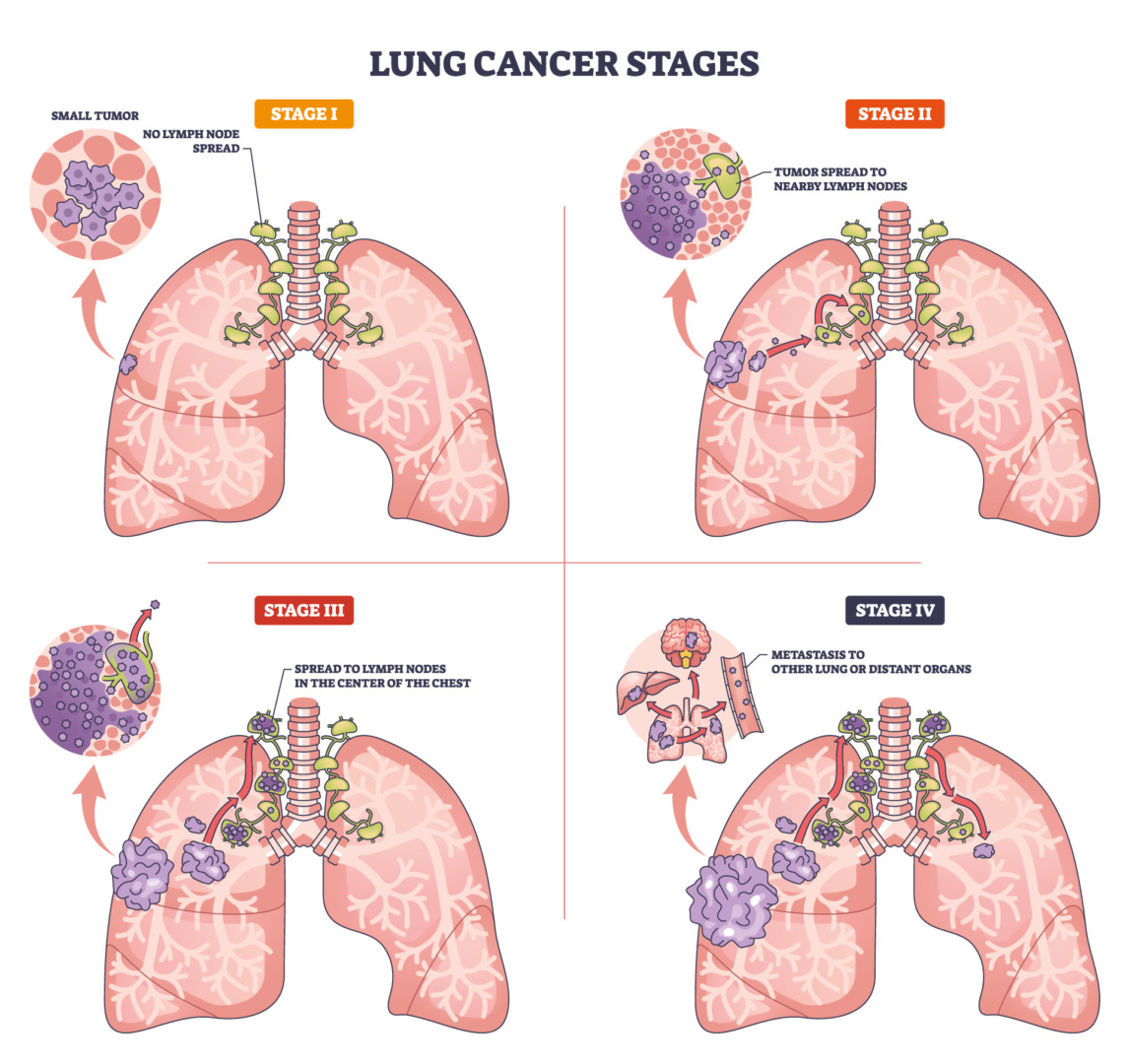
Stage 2 lung cancer means there is a lung tumour in one lung and that the cancerous cells may have reached nearby lymph nodes, but not distant organs such as the brain, liver or bones. It is often divided into Stage 2A and 2B based on tumour size and the lymph nodes involved.
The treating stage of lung cancer is crucial, as treatment options and prognosis depend on the specific stage at diagnosis.
Stage 2A, Stage 2B and TNM staging
Doctors use the TNM staging system to describe lung cancer precisely:
- T (Tumour): Describes the size of the primary tumour and how far it has grown into nearby tissue.
- N (Nodes): Indicates whether cancer cells are present in nearby lymph nodes.
- M (Metastasis): Confirms whether the cancer has spread (metastasised) to distant organs. For all Stage 2 cases, M is zero (M0), as there should be no distant spread.
The table below outlines the specific characteristics of Stage 2 lung cancer:
| Stage Subtype | Tumour (T) Characteristics | Lymph Node (N) Involvement | Distant Metastasis (M) | Key Implication |
| Stage 2A NSCLC | Moderate size (e.g. between 3 and 5 cm) | Either no lymph node involvement (N0), or cancer in the lymph nodes very close to the lung (N1) | M0 (No distant spread) | Considered a localised disease, often curable with surgery |
| Stage 2B NSCLC | Larger size (e.g. between 5 to 7 cm) | Cancer in the lymph nodes near the central airways in the centre of the chest (N2) | M0 (No distant spread) | Still a localised disease, often curable with surgery |
Note: Most patients with Stage 2 lung cancer have non-small cell lung cancer (NSCLC). Stage 2 small-cell lung cancer (SCLC) is less common, and its treatment pathway differs. Determining your exact lung cancer type, precise stage, and overall health is crucial for planning your treatment pathway.
Stage 2 Lung Cancer Symptoms and Red Flags
Some patients are diagnosed after an abnormal chest X-ray or CT scan done for another reason. Others come because of symptoms that have slowly worsened.
Common symptoms include:
- A cough that does not go away or that changes
- Coughing up blood or blood-stained phlegm
- Shortness of breath
- Chest pain, especially with deep breaths or coughing
- Repeated chest infections
- Unexplained weight loss, tiredness or loss of appetite
Fluid buildup in the chest, such as in pleural effusion, can affect the affected lung, leading to breathlessness and discomfort.
You should seek urgent medical attention if you cough up blood, have sudden severe shortness of breath or chest pain, or develop confusion, weakness or severe headaches. Not everyone with these symptoms has lung cancer, but they always deserve prompt assessment.
Causes and Risk Factors
In Singapore and worldwide, cigarette smoking remains the leading cause of lung cancer. Carcinogens in cigarette smoke damage lung tissue and can lead to the formation of cancerous cells, which is a key step in the development of lung cancer. The risk increases the more you smoke and the longer you have smoked, although many with the disease have never smoked.
Other contributors include second-hand smoke, prolonged exposure to air pollution or industrial fumes, previous chest radiotherapy and a family history of lung cancer. Having risk factors does not mean you will definitely develop cancer, and many with Stage 2 lung cancer have no apparent cause.
Early Detection and Screening
High-risk individuals, such as long-term smokers between the ages of 50 and 80, may be offered low-dose CT screening to detect lung cancer at an earlier stage than Stage 2. Screening is not suitable for everyone, but it can detect small tumours before symptoms appear, when treatment outcomes are often better.
If you have smoked heavily for many years or have other risk factors, you can discuss with your doctor whether screening is proper for you.
In Singapore, screening programmes are available through Neumark Lung & Chest Surgery Centre. Necessary scans and follow-ups are coordinated if an abnormality is found.

Diagnosis and Staging in Singapore
Most patients start with their family doctor, a polyclinic or a health screening centre that finds an abnormal shadow on the lungs. You may then be referred directly to a specialist, such as Neumark, for a full workup.
A typical assessment includes a detailed consultation and examination, chest CT scan and often a PET CT, and lung function tests to see if you are fit for Stage 2 lung cancer surgery. This might be followed by a biopsy performed by bronchoscopy or CT-guided needle biopsy. Pathologists will confirm the cancer type and may perform molecular tests to guide targeted therapies.
Staging Tests for Lymph Nodes and Brain
To confirm that Stage 2 lung cancer has not spread beyond the chest, additional tests may be needed. These include tests such as an endobronchial ultrasound (EBUS), which allows doctors to pass a thin scope down the breathing tubes and use ultrasound to guide a needle into mediastinal and hilar lymph nodes in the centre of the chest for accurate staging.
In some cases, a surgical procedure called mediastinoscopy is performed under general anaesthesia to sample mediastinal and hilar lymph nodes directly. A brain magnetic resonance imaging (MRI) scan is often recommended to rule out a silent spread to the brain, especially in patients with larger tumours or certain types of lung cancer.
These staging tests help ensure that Stage 2 lung cancer surgery is appropriate and that the cancer is truly confined to the chest, which in turn guides the overall lung cancer treatment plan.
At Neumark, Dr Harish personally reviews your scans and test results. When needed, he works and coordinates with radiologists, respiratory physicians and medical oncologists based at Gleneagles Hospital on Napier Road and Mount Alvernia Hospital on Thomson Road to finalise staging and plan your individual Stage 2 lung cancer treatment.
Stage 2 Lung Cancer Treatment Options
Lung cancer is treated using a combination of modalities tailored to the individual, based on the type, stage, and patient health, aiming to clear visible cancer in the chest and microscopic cancer cells that may have travelled elsewhere.
For most patients with non-small cell Stage 2 lung cancer (NSCLC) who are otherwise fit, the primary treatment is surgery to remove the tumour and the nearby lymph nodes, often followed by chemotherapy and, in selected cases, targeted or immune therapies.
Patients who can undergo surgery typically have good overall health and lung function, and no extensive cancer spread. The surgical goal is to remove all the cancer to minimise the risk of recurrence. A patient’s ability to tolerate surgery is the most significant factor in determining surgical suitability.

Types of Lung Surgery for Stage 2 Lung Cancer
The most common operation for Stage 2 lung cancer is a lobectomy, which removes the cancerous lobe of the lung containing the tumour along with nearby lymph nodes. The lung is divided into lobes: three on the right and two on the left. Most patients can tolerate losing one lobe without major long-term breathing problems.
In patients with limited lung reserve, perhaps from emphysema or previous lung disease, a less invasive operation called a segmentectomy or wedge resection may be considered. However, these are less commonly used for Stage 2 cancers because they remove less surrounding tissue. At the other end of the spectrum, there is the pneumonectomy, which removes an entire lung. This is rarely required but may be necessary for very large or centrally placed tumours that involve the central airway or major blood vessels.
During any lung resection, the surgeon aims for clear margins, meaning a rim of healthy tissue around the tumour with no cancer cells at the cut edge. If cancer is found at the edge of the removed tissue, additional treatment such as more surgery, radiotherapy, or a closer follow-up may be needed.
After lung cancer surgery, patients may have a chest tube to prevent fluid accumulation in the chest. If cancer has spread to lymph nodes near the other lung, this may indicate a more advanced stage and can influence the choice of surgery, radiation, or chemoradiation.
Molecular testing is also essential in the management of Stage 2 lung cancer. Testing for epidermal growth factor receptor (EGFR) mutations can help guide the use of targeted therapies, such as EGFR tyrosine kinase inhibitors, in selected patients.
When a diagnosis is first received, many patients immediately enter questions or terms such as “is Stage 2 lung cancer curable” or “lung cancer survival rates Stage 2” into a search engine. These are understandable worries. In practice, your outlook depends on several personal factors, and a specialist can put the statistics into context for you.
Neumark focuses on minimally invasive thoracic surgery. Whenever appropriate, Stage 2 lung cancer surgery is performed through minor cuts between the ribs using Video Assisted Thoracic Surgery (VATS), Uniportal VATS (U VATS) or Robot Assisted Thoracic Surgery (RATS). These approaches can reduce pain and shorten hospital stays compared with open surgery, while still allowing the careful removal of the tumour and lymph nodes.
Open surgery through a larger incision is needed if the tumour is large, involves major blood vessels, or when there are extensive internal scars.
Some patients are not fit for surgery because of other medical conditions, limited lung function, or personal choice. In these cases, radiotherapy alone or chemoradiotherapy can control the cancer in the chest and has been shown to improve outcomes for selected non-surgical Stage 2 NSCLC patients.

Radiotherapy Options for Stage 2 Lung Cancer
Radiation therapy, also known as external beam radiotherapy, directs high-energy rays at the tumour from outside the body. This procedure is carefully planned using CT scans to target the cancer while sparing as much healthy lung tissue as possible. Radiation therapy can shrink tumours and improve outcomes for patients who are not fit for surgery.
For patients who are not fit for surgery, a highly focused form of radiation therapy called stereotactic body radiation therapy (SBRT) can deliver very high doses in a small number of sessions and offers reasonable control for smaller Stage 2 tumours.
After a Stage 2 lung cancer surgery, routine radiation therapy is not usually given because surgery alone, with or without chemotherapy, is the standard of care. However, if cancer cells are found at the surgical margin, further surgery is not possible, and radiation therapy may be recommended to reduce the risk of the cancer coming back in the chest.
Radiation therapy is carefully planned to balance tumour control with lung preservation. Each patient’s breathing, lung function and the position of nearby organs are taken into account. Side effects can include tiredness, skin changes in the treated area, inflammation of the lung or oesophagus, and chest wall pain, especially for tumours near the chest wall. These are discussed and monitored throughout treatment by your specialist.
Systemic Therapies and Biomarker Testing
Chemotherapy remains standard after surgery for many Stage 2 non-small cell lung cancers (NSCLCs). It is usually given over three to four cycles to reduce the risk of the cancer returning. In some cases, chemotherapy or immunotherapy may be given before surgery, a strategy called neoadjuvant therapy, to shrink the tumour and make the operation easier, or to treat any microscopic spread early. The decision depends on the stage, the patient’s general health and the results of biomarker testing.
Biomarker testing examines biopsy tissue for specific gene changes, such as mutations in EGFR or rearrangements in ALK, and for proteins like PD-L1 that predict response to immune checkpoint inhibitors. Some patients with Stage 2 lung cancer may receive targeted tablets that block these genetic changes, or immunotherapy drugs that help the immune system attack cancer cells, as part of their lung cancer treatment, either before or after surgery.
Patients with certain features, such as lymph node involvement or specific molecular markers, have a significantly higher risk of recurrence and may benefit from additional therapies. These personalised treatments are most commonly used in higher-risk cases, for example, when lymph nodes contain cancer or when the tumour has certain molecular features.
Chemotherapy is typically platinum-based, meaning it includes drugs like cisplatin or carboplatin, combined with another agent. Specific regimens are tailored to each patient and discussed with your medical oncologist.

Clinical Trials and Emerging Treatments
Some patients with Stage 2 lung cancer may be suitable for clinical trials of new drugs or treatment combinations. Clinical trials are carefully designed research studies that test whether a new therapy is safe and effective, and are conducted under close monitoring with strict ethical oversight.
There are no guarantees that a trial drug will work better than standard treatment, but trials can offer access to promising therapies that are not yet widely available. Neumark works closely with medical oncologists who can advise on any open clinical trials in Singapore and whether you might be eligible based on your cancer type, stage, and test results.
Recovery, Follow Up and Prognosis
After minimally invasive Stage 2 lung cancer surgery, most patients stay in the hospital for around 3 to 5 days. You are encouraged to sit out of bed, walk, and start breathing exercises early to reduce the risk of complications. Adherence to national and international guidelines for follow-up care ensures excellence in patient management.
While recovering from lung cancer surgery, it’s normal to have some increased breathlessness during physical activity due to the removal of lung tissue. At home, many return to light activities within 2 to 3 weeks and feel close to their usual energy levels by 6 to 8 weeks, although this varies.

Stage 2 Lung Cancer Survival Rates and Prognosis
Lung cancer survival rates Stage 2 vary depending on whether the cancer is NSCLC or Stage 2 small cell lung cancer (SCLC), the exact Substage (2A or 2B), how many lymph nodes contain cancer cells, the patient’s general health and fitness, and whether all appropriate treatments, including surgery and systemic therapies, can be delivered.
Extensive studies suggest a 5-year survival rate of 50-60% for Stage 2 NSCLC, although rates are higher for Stage 2A and lower for Stage 2B. Newer treatments, including immunotherapy, are further improving outcomes. For Stage 2 small-cell lung cancer (SCLC), outcomes are generally poorer because the disease is more aggressive. However, early comprehensive treatment with chemotherapy, radiotherapy and surgery, when appropriate, makes a meaningful difference.
It is important to remember that survival statistics are based on groups of patients treated in the past and cannot predict what will happen to any individual.
Follow-up after Stage 2 lung cancer treatment typically includes regular clinic visits, periodic CT scans to check for recurrence, and monitoring for side effects of chemotherapy, targeted therapy or immunotherapy. Regular CT scans for several years after treatment are standard to monitor for recurrence in lung cancer patients.
Supportive Care and Living Well after Treatment
Managing symptoms and side effects is an essential part of recovery and long-term well-being. Common issues after Stage 2 lung cancer treatment include pain, breathlessness, fatigue, nausea from chemotherapy, peripheral nerve symptoms such as tingling in the hands or feet, and a persistent cough. Most of these improve over time. Your medical team can offer medications, adjustments to your treatment plan, and practical advice to help you feel more comfortable.
Pulmonary rehabilitation, a structured programme of exercise and education, can improve breathing, stamina and confidence after lung surgery or radiotherapy. Physiotherapists, dietitians and smoking cessation specialists all play a role in helping you regain strength and reduce the risk of further lung problems. If you still smoke, quitting at any stage improves your response to treatment and your overall health. Support for smoking cessation is also available through Neumark.
Psychological and emotional support for patients and families is equally important. A cancer diagnosis can be overwhelming, and feelings of anxiety, sadness or uncertainty are normal. Counselling, support groups and open conversations with your medical team can help you and your loved ones navigate the experience.
Palliative care, which focuses on improving quality of life and managing symptoms, can be involved early in your treatment journey, not only at the very end of life. Palliative care specialists work alongside your surgeon and oncologist to ensure you remain as comfortable and active as possible throughout your Stage 2 lung cancer treatment and beyond.
Why Choose Neumark
Neumark Lung & Chest Surgery Centre focuses on minimally invasive thoracic surgery, including VATS, U-VATS and RATS procedures for Stage 2 lung cancer. Dr Harish Mithiran has extensive experience in lung resections and lymph node dissections. He works closely with medical oncologists, respiratory physicians and radiologists based at Gleneagles Hospital and Mount Alvernia hospitals. Neumark also provides practical help with arranging diagnostic tests, liaising with insurance for pre-authorisations, and scheduling surgery and chemotherapy around your work and family commitments.
For patients in Singapore, working with a private lung cancer treatment centre means rapid access to diagnostic imaging and biopsies, coordinated treatment planning in a single centre, surgery, systemic therapies, and follow-up arranged around work and family commitments.
To discuss personalised Stage 2 lung cancer treatment and whether minimally invasive lung cancer surgery is suitable for you, contact Neumark for a consultation with Dr Harish Mithiran.

