Neumark Lung & Chest Surgery Centre in Singapore specialises in Uniportal Video-Assisted Thoracoscopic Surgery (U-VATS) for lung nodules, an advanced surgical method with multiple benefits over traditional approaches. This precise procedure is ideal for removing benign and malignant pulmonary nodules and requires only a single small incision.
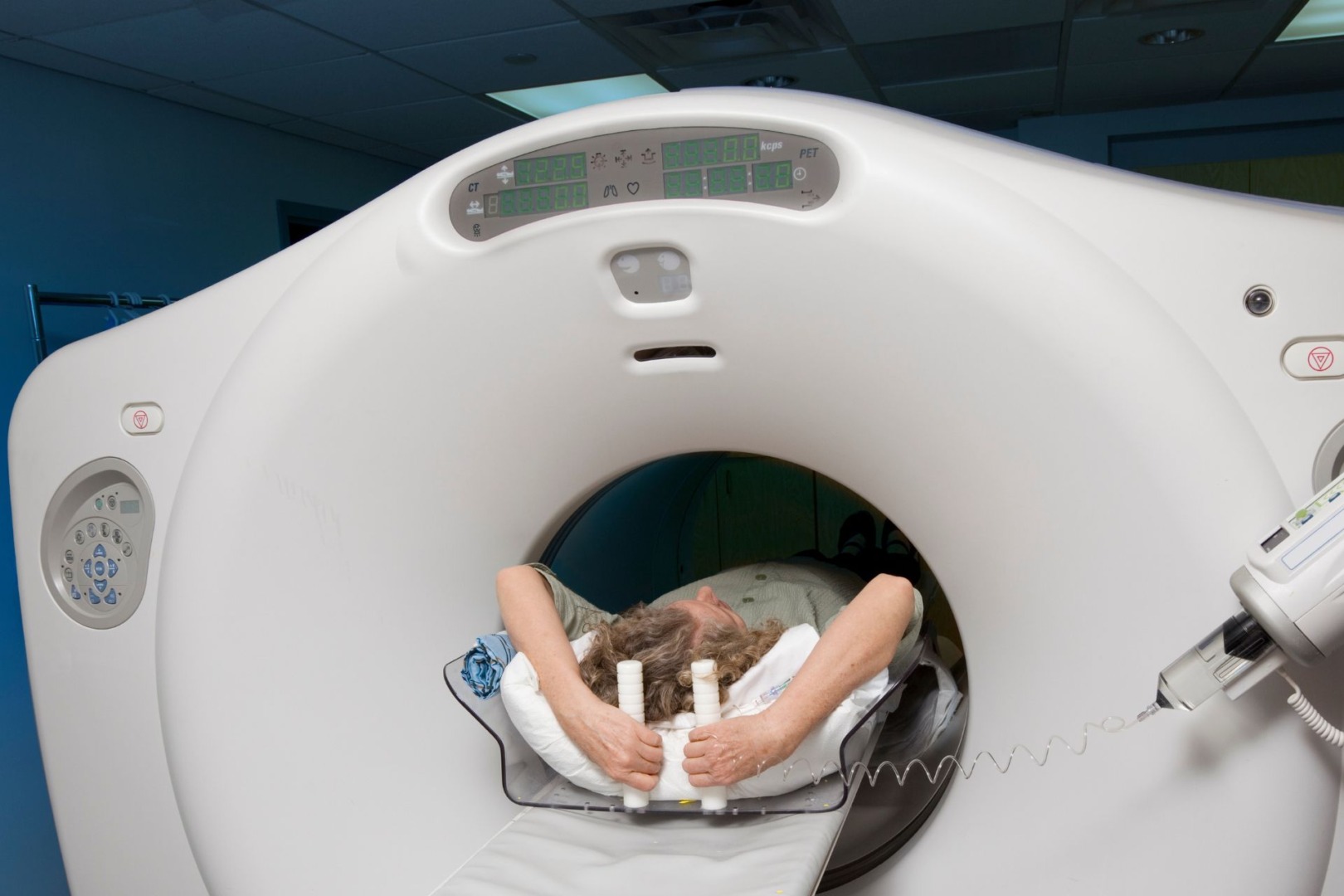
A lung nodule is a small, round, or oval-shaped growth in the lung tissue, typically less than 3 centimetres in diameter. These white spots on the lungs are usually detected incidentally during imaging tests, such as chest X-rays or CT scans for other chest conditions.
Various factors, such as infections, inflammation, benign tumours, or scar tissue, can cause lung nodules. While the majority of lung nodules are benign or non-cancerous, some can be early signs of lung cancer. If you’re concerned about lung nodules, contact a healthcare professional to evaluate them and determine their nature and whether further monitoring or testing is necessary.
U-VATS represents a significant advancement in thoracic lung nodule removal surgery. This technique utilises a single small incision, typically 3-4 centimetres, through which the entire surgical procedure is performed. This approach offers significant advantages over multi-portal VATS, which uses several small cuts. It represents a significant step forward in treating lung conditions effectively while minimising patient discomfort and recovery time, offering several advantages over traditional multi-portal VATS or open thoracotomy:
- Reduced invasiveness: The single incision minimises trauma to the chest wall.
- Decreased postoperative pain: Patients often report less discomfort following U-VATS.
- Faster recovery: Many patients experience shorter hospital stays and quicker return to normal activities.
- Improved cosmetic outcomes: The single, small incision results in minimal scarring, supporting psychological recovery following surgery.

Neumark’s surgeons work with precision and care in a U-VATS lung nodule procedure. We insert a high-definition camera through the small incision, giving us a clear view of the lung on a monitor. Using specialised instruments, we can then remove the nodule with remarkable accuracy. This approach allows us to access the thoracic cavity effectively while minimising patient discomfort.
While U-VATS has many benefits, we understand that every patient’s case is different. Sometimes, a traditional thoracotomy is the better option, like during an emergency when a nodule blocks an airway. This open surgery technique uses a longer incision on the chest side, allowing quicker direct visual access to the lungs.
Our services extend beyond surgery. Neumark offers comprehensive consultations for patients with lung nodules or lesions detected on imaging scans, helping them understand their condition and options. During these consultations, we carefully assess the lung mass, discuss potential risks, provide a prognosis, and outline all available lung nodule treatment options, helping you find the best path forward.
Following your lung nodule CT scan, we will schedule a follow-up appointment with our thoracic specialist to review the results. We’ll take the time to answer all your questions and ensure you fully understand the findings. Unlike in many other places worldwide, most people in Singapore are eligible for lung screenings. That’s why we strongly encourage early screening to detect lung cancer at its earliest, most treatable stages.

No matter the size of your lung nodule, Neumark’s experienced thoracic surgeons will develop a tailored monitoring plan. For most patients, this involves regular follow-up appointments to monitor the nodule’s growth or changes over time. These check-ups serve two crucial purposes: they allow us to detect any signs of lung cancer early and provide reassurance if the nodule remains benign.
Neumark’s preferred method, uniportal video-assisted thoracic surgery (U-VATS), is a leading technique for removing pulmonary nodules. This advanced approach offers a less invasive option with minimal incisions, promoting faster recovery and reduced post-operative discomfort. It’s one way we’re working to improve outcomes and experiences for our patients with lung nodules. We understand that potentially cancerous growths often require swift action. We’re prepared to intervene promptly with appropriate surgical measures to protect your health and safety.

