For many, the discovery of a mediastinal tumour can be overwhelming, understandably. It’s normal for patients to have countless questions about treatment options and outcomes. Fortunately, advances in thoracic surgery have revolutionised how we approach these complex cases, providing patients with peace of mind. Much of this is thanks to Video-Assisted Thoracoscopic Surgery (VATS), which has emerged as the gold standard for many mediastinal conditions.
Benign or Malignant Mediastinal Tumours
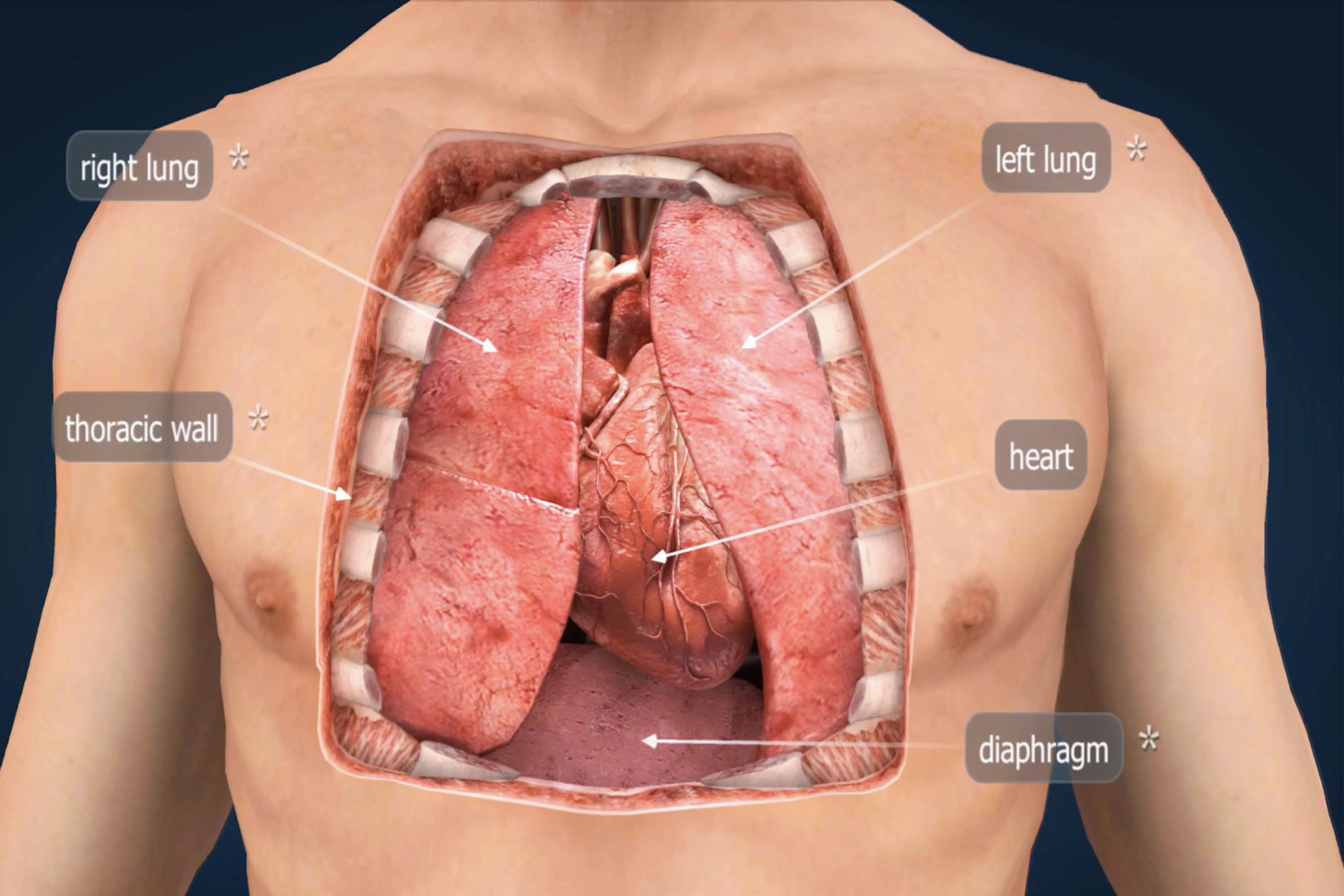
The mediastinum, the central compartment of the chest cavity situated between the lungs, houses vital structures, including the heart, major blood vessels, the oesophagus, and the thymus gland. When tumours develop in this critical region, they require expert evaluation and often surgical intervention.
Mediastinal tumours encompass a diverse group of growths that can be benign or malignant, arising from various tissues within the chest cavity. The most common types include thymomas, thymic carcinomas, lymphomas, neurogenic tumours and mediastinal cysts. Each type presents unique challenges and requires tailored treatment approaches.
Many patients discover their mediastinal tumour incidentally during routine chest imaging for unrelated conditions. In some cases, patients may experience symptoms such as chest pain, shortness of breath, coughing, or difficulty swallowing. Some tumours, particularly thymomas, can be associated with myasthenia gravis, an autoimmune condition affecting muscle strength.
The location and characteristics of mediastinal tumours make them particularly challenging to treat through traditional open surgery. Historically, accessing these tumours required large incisions through the chest wall or sternum, resulting in significant post-operative pain, extended recovery periods, and increased risk of complications.
Related Mediastinal Conditions
What Is Minimally Invasive Thoracic Surgery?
Video-assisted thoracoscopic surgery (VATS) is a technique that utilises small incisions, typically ranging from 5mm to 3cm, through which a tiny camera, called a thoracoscope, and specialised instruments are inserted. The high-definition camera on the thoracoscope provides surgeons with magnified, detailed views of the surgical field, often superior to what’s achievable through traditional open approaches.
VATS for mediastinal tumours has gained widespread acceptance due to its numerous advantages over conventional surgery. The smaller incisions result in less tissue trauma, reduced blood loss, decreased post-operative pain, and faster recovery times. For this same reason, patients typically experience shorter hospital stays and can return to normal activities more quickly than those undergoing traditional open procedures.

The VATS Procedure for Mediastinal Tumours
The surgical approach for VATS varies depending on the tumour’s location, size and its relationship to the surrounding structures. Most procedures are performed under general anaesthesia with single-lung ventilation, allowing the affected lung to collapse, providing optimal visualisation of the mediastinal space.
During the procedure, the surgeon creates several small incisions strategically positioned to provide the best access to the tumour. The thoracoscope is inserted through one incision, whilst surgical instruments are introduced through the others. This multi-port approach allows for precise manipulation of tissues while maintaining excellent visualisation throughout the operation.
For anterior mediastinal masses located near the front of the chest, such as thymomas, the surgeon can achieve complete thymectomy through VATS, carefully dissecting the tumour and surrounding thymic tissue whilst preserving vital structures. The procedure requires meticulous attention to anatomical planes and potential adhesions to nearby organs.
Posterior mediastinal tumours, often neurogenic in origin, present different challenges due to their proximity to the spine and major vessels. VATS techniques also allow surgeons to approach these lesions with minimal disruption to surrounding tissues, often achieving complete resection with excellent functional outcomes.

Benefits and Outcomes of VATS
The advantages of VATS for mediastinal tumours extend beyond the immediate surgical period. Research consistently demonstrates superior outcomes compared to traditional open approaches, with reduced post-operative complications, shorter hospital stays, and improved patient satisfaction.
Pain management represents one of the most significant benefits of minimally invasive surgery. The smaller incisions and reduced tissue trauma result in considerably less post-operative discomfort, often allowing patients to mobilise earlier, requiring fewer pain medications. This enhanced recovery profile translates to improved quality of life during the healing process.
Cosmetic outcomes are also better with the VATS approach, as the small, strategically placed incisions heal to form minimal scars. This consideration is particularly important for younger patients or those concerned about visible surgical marks, and can have a significant psychological impact during recovery.
The long-term oncological outcomes for malignant mediastinal tumours treated with VATS have similar survival rates to open surgery. Some studies do suggest that there are improved outcomes with VATS due to the ability to commence adjuvant treatments sooner when indicated.

Patient Selection and Considerations
Not all mediastinal tumours are suitable for VATS treatment, but many are. Patient selection requires a careful evaluation of multiple factors, including tumour size, location, relationship to vital structures and the patient’s overall health status. Individual patient factors such as previous chest surgery, significant pleural adhesions, or severe cardiac or pulmonary conditions may influence surgical planning.
The technique is most commonly used for:
- Thymomas
- Benign cysts (e.g., bronchogenic or pericardial cysts)
- Neurogenic tumours
- Select cases of lymphoma and germ cell tumours (mainly for biopsy or diagnostic purposes)
The decision to proceed with VATS is made based on tumour size, location, involvement with nearby structures, and the patient’s overall health. Advanced imaging studies, including CT and MRI scans, help surgeons determine the feasibility of minimally invasive approaches. In some cases, Robotic-Assisted Thoracic Surgery (RATS) may be considered for added dexterity in complex areas.
Large tumours, or those with extensive adhesions to surrounding structures, may require switching to open surgery during the procedure. Experienced thoracic surgeons ensure low conversion rates through careful pre-operative planning and advanced VATS techniques.
A thorough pre-operative assessment ensures optimal patient selection and preparation for surgery.

Recovery and Follow-up Care
Recovery from VATS for mediastinal tumours typically proceeds more smoothly than traditional open surgery. Most patients remain in the hospital for 2 to 4 days, depending on the complexity of the procedure and their progress in recovery. Early mobilisation is encouraged, with many patients often walking within hours of surgery.
Post-operative care focuses on pain management, respiratory physiotherapy, and monitoring for complications. The reduced invasiveness of VATS often allows patients to return to desk-based work within 1-2 weeks and resume normal activities within 4-6 weeks, significantly faster than recovery from open procedures.
Long-term follow-up remains essential, particularly for patients with malignant tumours. Regular imaging studies and clinical assessments help detect any recurrence early and ensure optimal long-term outcomes.

Make an Informed Decision
If you’ve been diagnosed with a mediastinal tumour, it’s essential that you work with an experienced thoracic surgeon to ensure the best possible outcome. The complexity of these cases requires specialist knowledge and technical expertise in advanced minimally invasive techniques, which can only be provided by an experienced and trusted thoracic surgeon.
The team at Neumark Lung & Chest Surgery Centre combines extensive expertise in minimally invasive techniques with compassionate, patient-centred care. Contact Neumark today to arrange a comprehensive consultation. Our specialists will evaluate your case, explain all available treatment options, and guide you towards the most appropriate surgical approach for your specific needs.

