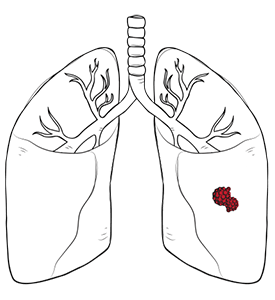

A pneumothorax is a medical condition characterised by the partial or complete collapse of one or both lungs. This occurs when air escapes from the lung into the pleural cavity, the space between the lung and the chest wall. Once air enters this cavity, it exerts pressure on your lungs, making it difficult, or even impossible, for the lungs to expand during inhalation. As the pressure builds, the lung may collapse further, creating a problem that compromises respiratory function and requires prompt medical attention.
The air typically enters this space through a rupture in the lung tissue, such as a burst blister or bullae. This rupture can happen spontaneously or due to trauma, lung disease, or surgical complications. The severity of pneumothorax can range from mild and asymptomatic to life-threatening, depending on the cause and the volume of air trapped in the pleural space.
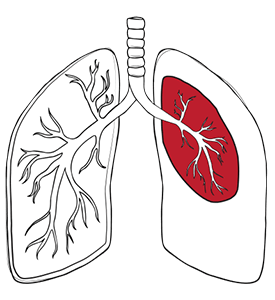
When the integrity of the pleural space is compromised, air enters and exerts pressure on the lung, preventing it from fully expanding and contracting. In the case of a tension pneumothorax, the situation becomes even more critical: a one-way valve effect develops, allowing air to enter the pleural cavity but not escape. This leads to rapidly increasing pressure within the chest, further collapsing the lung and potentially shifting the mediastinum, which can impair heart and lung function.

Symptoms of pneumothorax can vary depending on the size and cause of the air leak. Common signs include sudden chest pain, which may be sharp or stabbing, and shortness of breath. Individuals may also experience rapid breathing, fatigue, or a feeling of tightness in the chest. In more severe cases, symptoms can escalate to include cyanosis (bluish skin), hypotension, and altered consciousness, signalling respiratory distress or cardiovascular compromise. If you have sudden chest pain or difficulty breathing, seek medical attention immediately. Recognising pneumothorax symptoms early is critical to timely intervention.

There are multiple types of pneumothorax, each with distinct causes:
Diagnosis begins with a thorough clinical examination and symptom assessment. Physical examination can reveal key signs, including reduced or absent breath sounds on the affected side, detected through auscultation; hyper-resonant percussion sounds, which suggest air in the chest cavity; and observable respiratory distress, such as rapid breathing, difficulty breathing, and chest pain.
Imaging will confirm the diagnosis, with chest X-ray as the initial step to reveal lung collapse and pleural air presence. CT scans provide detailed anatomical insight in subtle cases, identify underlying lung disease, locate air leaks, and detect complications. In emergencies, such as tension pneumothorax, clinical diagnosis takes precedence due to the urgency of intervention.
Symptoms can range from subtle to severe, depending on the severity of the air leak. Sudden chest pain and breathing difficulty require immediate medical attention to prevent serious complications.
While many cases of pneumothorax resolve with appropriate treatment, there are potential complications that can pose significant risks.
A tension pneumothorax is particularly dangerous, as the trapped air in the pleural space can rapidly increase pressure, leading to severe cardiovascular compromise, obstructive shock, or even cardiac arrest.
Other complications of pneumothorax include the spread of air to different areas, such as the mediastinum (pneumomediastinum), the pericardium (pneumopericardium), or the abdominal cavity (pneumoperitoneum). In some cases, a pneumothorax can result in long-term lung damage or increase the risk of future episodes, especially if there is underlying lung disease.

At Neumark Lung & Chest Surgery Centre, the preferred surgical approach for recurrent or persistent pneumothorax is uniportal video-assisted thoracic surgery (U-VATS). This advanced technique allows surgeons to access the thoracic cavity through a single small incision, resulting in reduced pain, quicker recovery times, and minimal scarring.
During U-VATS, the thoracic surgeon removes the damaged area of the lung responsible for the air leak, such as bullae or blebs. To further reduce the risk of recurrence, a procedure called pleurectomy may be performed. In this technique, the surgeon removes part of the pleura (the lining around the lung), encouraging the lung to adhere to the chest wall. These adhesions help prevent future episodes by eliminating the space where air could accumulate.
This combination of bullae resection and pleurectomy has proven effective in reducing recurrence rates, particularly in patients with spontaneous pneumothorax.

Following pneumothorax treatment, patients typically experience improved breathing and comfort. Pain management is individualised, and early mobilisation supports lung re-expansion. Hospital observation is standard after chest tube placement or surgical intervention.
The recovery outlook depends on the underlying cause and the associated lung disease. Patients with primary spontaneous pneumothorax generally recover well, with full lung re-expansion and no lasting effects. Secondary spontaneous pneumothorax or trauma-related cases may have more complex recovery and higher recurrence risk.
Post-discharge care includes regular follow-ups and chest imaging to ensure proper lung expansion and monitor for recurrence. Patients must avoid activities that increase pressure, such as air travel and scuba diving, for a specified period of time. Smoking cessation is crucial for reducing the risk of recurrence and promoting lung health.
With appropriate treatment and ongoing care, most patients return to their normal activities and maintain a good quality of life, taking steps to prevent future episodes.

Preventing recurrence is a central goal of pneumothorax management. In addition to surgical solutions, lifestyle modifications play an important role. Quitting smoking, maintaining healthy lung function through regular exercise, and managing underlying respiratory conditions like asthma or COPD are key components of long-term pneumothorax prevention.
Patients with secondary spontaneous pneumothorax linked to chronic lung disease must work closely with their healthcare provider to manage their primary condition. Addressing contributing factors such as infections, inflammation, or genetic disorders can significantly improve outcomes and reduce future risks.

Pneumothorax is a serious condition that can severely impact respiratory function and overall health. Whether caused by trauma, lung disease, or occurring spontaneously, early diagnosis and effective pneumothorax treatment are essential. At Neumark Lung & Chest Surgery Centre, we specialise in the evaluation and management of pneumothorax using state-of-the-art technology and minimally invasive surgical methods.
Our team, led by Dr Harish Mithiran, provides tailored pneumothorax treatments designed to minimise complications and prevent recurrence. If you or a loved one is experiencing pneumothorax symptoms or has been diagnosed with a lung condition, contact us at Neumark for a comprehensive consultation.
Pneumothorax may occur as a complication following chest tube removal. Air entering the pleural space during chest tube removal is especially common in patients with relatively thin, muscular chest wall anatomy. Even after successful thoracoscopic treatment, there is still a risk of recurrence due to poor healing or the formation of a new blister (bullae) in the lung.
Pneumothorax is when air accumulates between the lung and chest wall, causing the lung to collapse. This can be caused by trauma or underlying medical conditions such as COPD and can also occur spontaneously without any underlying disease. Increased air inside the chest cavity can cause an increase in pressure that pushes against the heart and lungs, reducing blood flow throughout your body. This is a sign of tension pneumothorax. It typically requires immediate medical attention as it can be life-threatening if left untreated.
The treatment for spontaneous pneumothorax can vary depending on the severity of the condition. In general, conservative treatment may be recommended for mild to moderate cases. At the same time, minimally-invasive interventions such as U-VATS may be prescribed if the air leak does not heal by itself and is prolonged, the pneumothorax recurs the second time, there is the presence of bilateral pneumothorax (pneumothorax occurring in both the lungs at the same time) and for professionals who are working as pilots, cabin crew staff and divers who are at a higher risk of pneumothorax recurrence due to pressure changes affecting their lungs during their work.
Secondary spontaneous pneumothorax occurs due to an underlying lung condition such as chronic obstructive pulmonary disease, cystic fibrosis, asthma or pneumonia. Air can leak from the lung into the chest wall, causing one side of the chest to collapse, leading to severe breathing difficulties. Treatment may involve inserting a tube to remove excess air from the pleural cavity and surgery to repair any damage.
Pneumothorax can occur after a transthoracic lung biopsy. Lung biopsies involve taking tissue samples from the lungs to identify any underlying medical conditions or other abnormalities. The dysfunction can happen when air escapes into the chest cavity during the procedure and causes the biopsied lung to collapse. The risk increases if the patient already has COPD or emphysema since these diseases weaken the lungs making them more likely to rupture during a biopsy.
A collapsed lung can be a complication of any chest cavity surgery. The condition is rare and usually only occurs in cases with underlying respiratory issues or complications with anaesthesia.
DISCLAIMER: The information provided on this website is for general informational purposes only and is not intended as a substitute for professional medical advice, diagnosis, or treatment. The use of this website does not create a doctor-patient relationship and no medical advice should be inferred or assumed. It is the user’s sole responsibility to seek the advice of their healthcare professionals for any medical concerns they may have and the user should not disregard, or delay, prompt medical advice for any such condition.
Neumark Lung and Chest Surgery Centre benefits from the expertise of a multidisciplinary team led by Dr Harish Mithiran, senior consulting thoracic surgeon at Gleneagles Hospital and Mt Alvernia Hospital.
Neumark is a lung and chest specialist centre with access to leading treatment modalities to achieve the best possible outcomes for lung disease and preventative patient screening.
Our foremost priority is to treat your condition as effectively as possible. Schedule a private consultation today; complete the form below, call, +65 6908 2145; WhatsApp, +65 9726 2485; or email, info@neumarksurgery.com.
Gleneagles Medical Centre
6 Napier Road
#02-09 Gleneagles Medical Centre
Singapore 258499
Mount Alvernia Hospital
820 Thomson Road
#06-07 Medical Centre A
Singapore 574623