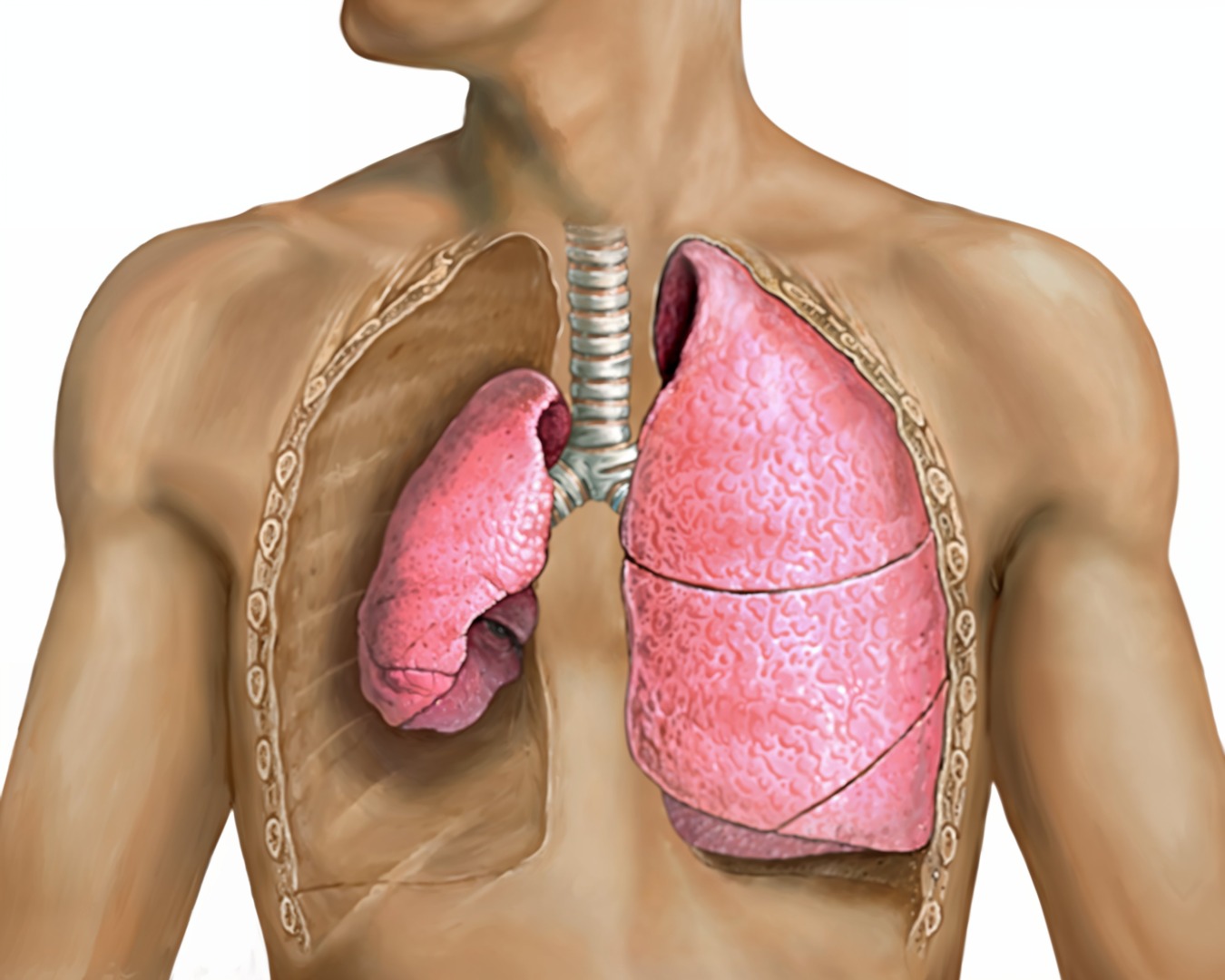
The health of our lungs determines a lot about the quality of our living days. This is why thoracic surgeons are continually looking for better ways to help their patients and their lungs. Thankfully, there have been exciting breakthroughs that can help many people, such as Uniportal Video-Assisted Thoracic Surgery, or U-VATS for short. It’s making a difference in the treatment of pneumothorax, a condition where air enters the space between the lung and chest wall, causing lung collapse. Thanks to U-VATS, pneumothorax can now be addressed more efficiently and with less patient discomfort.
At Neumark Lung & Chest Surgical Centre, our team has embraced U-VATS as a primary method for treating pneumothorax. This approach offers substantial benefits over traditional surgical methods, improving the procedure and patient recovery.
Understanding Pneumothorax
Pneumothorax occurs when air enters the space between the lung and chest wall. This can be very dangerous as there is a delicate balance of pressure within the body. “Unwanted’ air can lead to severe complications. But what exactly causes the air to enter this space? There are two types of pneumothorax: spontaneous and traumatic pneumothorax. It can either occur spontaneously, or as a result of trauma.
Spontaneous pneumothorax has additional categories, including primary and secondary spontaneous pneumothorax. Primary spontaneous pneumothorax typically affects young, tall, thin males without apparent lung disease, while secondary spontaneous pneumothorax occurs in individuals with underlying lung conditions.
Traumatic pneumothorax, as the name suggests, is caused by injury to the chest. Regardless of the cause, the consequences can be severe, ranging from mild discomfort to life-threatening respiratory distress.
Traditionally, the management of pneumothorax has involved more invasive procedures, such as chest tube insertion or open thoracotomy. However, these methods often result in more extended hospital stays, increased pain, and a higher risk of complications. The introduction of U-VATS has marked a significant improvement in treating this condition, reducing recovery times and lowering risk.
The U-VATS Advantage
Uniportal video-assisted thoracic surgery is at the cutting edge of minimally invasive thoracic procedures. U-VATS has become the preferred method at Neumark for treating primary spontaneous pneumothoraces and managing traumatic and recurrent cases. The procedure’s key advantage lies in its minimally invasive nature, which provides numerous patient benefits. To understand why the benefits of U-VATS are so high, it’s important to understand what happens during the procedure.

During a U-VATS procedure, the surgeon makes a single small incision in the chest wall, typically about 2-3 centimetres long. This single port serves as the entry point for surgical instruments and a high-definition camera. The camera provides the surgeon with a magnified, clear view of the inside of the chest cavity, displayed on monitors in the operating room. This enhanced visualisation allows for precise identification and treatment of the underlying cause of the pneumothorax.
The primary goal of the U-VATS procedure in pneumothorax cases is to identify and remove the leaking blister, or bullae, on the lung surface. These blisters are often the source of air leakage, leading to lung collapse. By removing these weakened areas, surgeons can effectively prevent further air leakage and reduce the risk of recurrence.
Benefits of U-VATS for Pneumothorax
The adoption of U-VATS for pneumothorax treatment offers several significant advantages over traditional methods:

- Reduced Pain: The single, small incision results in less postoperative pain than open procedures or multi-port VATS.
- Faster Recovery: The recovery time with VATS surgery for pneumothorax is typically much faster than other methods. Patients usually experience shorter hospital stays and quicker return to normal activities.
- Improved Cosmetic Outcome: The single small incision leaves a minimal scar. This small psychological effect can have a marked difference in a person’s quality of life.
- Lower Risk of Complications: The minimally invasive procedure reduces the risk of surgical site infections and other complications.
- Excellent Visibility: The high-definition camera provides superior surgical field visualisation, allowing for precise treatment.
- Effective Treatment: U-VATS has shown high success rates in treating pneumothorax and preventing recurrence.
Expertise at Neumark Lung & Chest Surgical Centre
At Neumark Lung & Chest Surgical Centre, the thoracic specialist team led by Dr Harish Mithiran brings a wealth of experience and expertise to treating pneumothorax and other lung diseases. As a senior consultant thoracic surgeon at Gleneagles and Mount Alvernia Hospitals, Dr Mithiran has been at the forefront of adopting and refining minimally invasive techniques like U-VATS.
Neumark’s approach to patient care goes beyond technical expertise. Their guiding principle combines personalised care coordination, sound clinical knowledge and groundbreaking treatments. This holistic approach ensures that each patient receives tailored treatment plans for the best possible outcomes. If you or a loved one is living with pneumothorax, consider calling Neumark today to hear about how U-VATS can give your lungs the support they deserve.

