Understanding Funnel Chest Syndrome
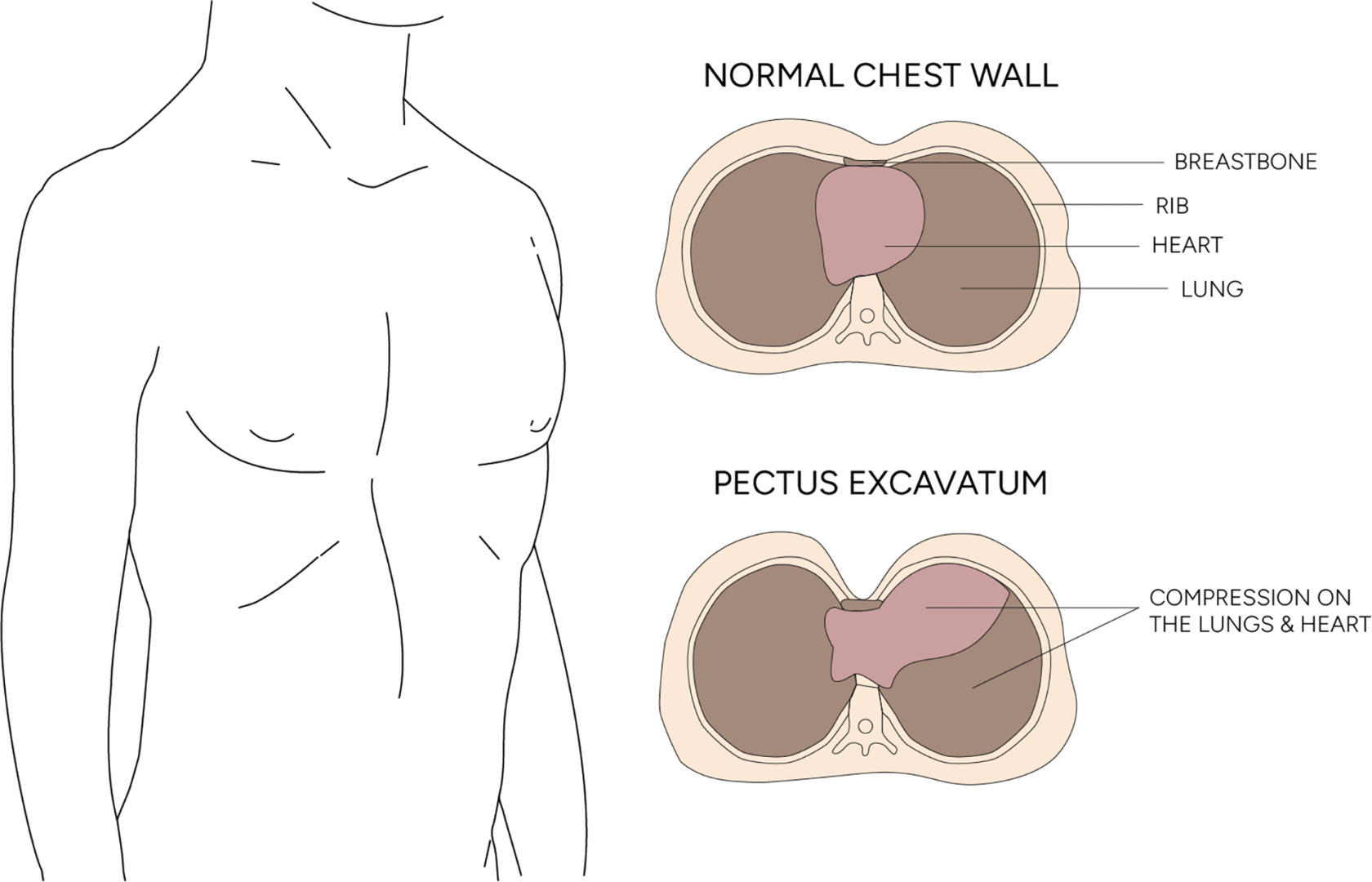
Funnel chest, also known as pectus excavatum or sunken chest, is the world’s most common chest wall deformity. It occurs in approximately 1 in 300 to 400 live births and is 3 to 4 times more prevalent in males than females. The condition involves an inward depression of the sternum (breastbone) and adjacent ribs, resulting in a concave or ‘funnel-shaped’ appearance of the anterior chest wall.
For many with funnel chest syndrome, the physical manifestation is just one part of the condition that has far-reaching physiological implications. The severity varies greatly, from barely noticeable cosmetic depressions to deep indentations that can displace internal organs and restrict cardiopulmonary function.
Most patients notice the depression in early childhood, but the condition becomes more pronounced during adolescent growth spurts when the chest wall is growing rapidly. This timing adds another layer of complexity as physical changes occur, and young people are most sensitive about body image and peer pressure. Even mild cases of funnel chest can cause significant emotional distress.
Funnel Chest Causes
The exact cause of funnel chest is still unknown, but several theories with scientific backing exist. Most prominently, genetic factors play a significant role, with about 40% of patients having a family history of chest wall deformities. This genetic predisposition suggests an inherited connective tissue abnormality that affects cartilage development and chest wall formation.
Intrauterine positioning has also been proposed as a possible contributing factor in the development of funnel chest, particularly in cases without a clear genetic link. Constricted fetal positioning may exert pressure on the developing sternum, potentially creating the first stages of chest wall deformity. While this theory remains speculative, it offers some plausible explanations.
The biomechanical theory suggests that overgrowth of costal cartilage puts pressure on the sternum and pushes it inwards during development. This overgrowth is due to a condition that affects cartilage development, such as abnormal chondrocyte function or disrupted cartilage metabolism.
Strong clinical evidence links pectus excavatum with connective tissue disorders such as Marfan syndrome, Ehlers-Danlos syndrome and osteogenesis imperfecta. These conditions affect collagen production and the structural integrity of connective tissue, increasing susceptibility to chest wall abnormalities.

Diagnostic Tests
Diagnosing pectus excavatum typically begins with a physical examination and reviewing the patient’s medical history. The funnel chest appearance – characterised by a sunken sternum that creates a hollow in the middle of the chest – is unmistakable to clinicians. In severe cases, asymmetry may be present, with one side of the chest more depressed. The deepest part of the depression is usually at the junction of the sternum and xiphoid process (the pointed end of the sternum), with the surrounding rib cartilages angled abnormally.
Several imaging tests may be performed to confirm the diagnosis and assess the severity of the condition. Chest X-rays, CT scans and MRI scans provide detailed images of the chest wall to visualise the extent of the deformity.
Pulmonary function tests are essential for assessing lung function and detecting respiratory issues. Cardiac tests, such as echocardiograms and electrocardiograms, are also used to evaluate heart function and detect cardiac abnormalities. A comprehensive evaluation is necessary to develop a treatment plan tailored to the patient.

When to Seek Medical Attention for Funnel Chest
The implications of funnel chest extend beyond aesthetics. In moderate to severe cases, the depressed sternum can compress cardiac structures, especially the right ventricle, and reduce cardiac output during exercise. This manifests as decreased stamina, fatigue during exercise, and sometimes cardiac arrhythmias. In addition, sometimes, the condition can displace the heart and result in cardiac issues like a leaky heart valve.
Pulmonary function may also be affected. A restricted chest cavity can limit lung expansion, reducing total lung capacity and exercise performance. Many patients report shortness of breath during physical activity, even when other clinical tests are standard.
In some cases, pectus excavatum can cause pulmonary hypertension, a condition in which the blood pressure in the lungs is high. Key symptoms include a noticeable indentation in the chest, shortness of breath, chest pain, fatigue during physical activity, palpitations, and a rapid heartbeat. This condition necessitates early treatment to prevent long-term damage to the heart and lungs, allowing patients to maintain optimal cardiopulmonary function.
Just as important is the psychological impact. Studies show higher rates of body image concerns, social anxiety and reduced quality of life in people with visible chest wall deformities. Young people often report avoiding activities that might expose their chests, such as swimming, which can severely impact their social development and self-confidence. If your child is experiencing any of these, it is worth exploring pectus excavatum treatment.

Nuss Procedure for Pectus Excavatum Treatment
The Nuss procedure has changed the landscape of funnel chest surgery. This minimally invasive technique has largely replaced the traditional Ravitch procedure, which involved extensive cartilage resection and sternal osteotomy.
The Nuss procedure works differently. Instead of removing abnormal cartilage, it remodels the chest wall through internal bracing. Under thoracoscopic guidance, the thoracic surgeon makes small lateral incisions through which a custom-shaped concave titanium bar is inserted behind the sternum. These small incisions under each arm allow specialised tools and a fibre optic camera to correct the position of the breastbone without making larger cuts in the chest. Once in place, the bar is rotated 180 degrees, and the depressed chest wall is instantly elevated to a normal contour.
This advanced solution has several advantages over the Ravitch procedure: smaller incisions, shorter operating time, minimal blood loss and preservation of the costal cartilage. The bar remains in place for 2-3 years before being removed through a minor procedure.
As with any surgical intervention, patient selection is key. The ideal candidate is typically between 12 and 18 years old, when the chest wall is most pliable. However, it can also be helpful for adults. A comprehensive preoperative evaluation includes CT imaging to measure the Haller index (the ratio of the transverse chest diameter to the anteroposterior diameter), pulmonary function testing and cardiac evaluation.

Recovery and Outcomes
Recovery from the Nuss procedure requires careful management and attention to detail.
Most patients can return to light activities within 3-4 weeks. Contact sports and heavy lifting are usually restricted for 3-6 months to prevent bar displacement. The bar is invisible, mainly beneath the skin, although patients are advised to carry medical alert information for situations such as security screenings at airports. There may also be initial postoperative pain as the chest wall adjusts to its new position.
Long-term outcomes are generally excellent. More than 90% of patients achieve good cosmetic results, significantly improving both physiological measures. Cardiopulmonary function usually improves, especially in those with preoperative compression.
The psychological benefits are just as compelling. Research consistently shows improvements in self-esteem, body image, and social confidence after successful chest wall repair. For many, these quality-of-life benefits often outweigh the medical considerations in patient satisfaction surveys.

Seeking Specialist Care
Funnel chest syndrome is more than an aesthetic concern. It encompasses a spectrum of physical and psychological implications that need to be considered and, in many cases, addressed through intervention.
While surgical repair of pectus excavatum can be effective, it comes with some risks and complications, as with any surgical intervention. It’s important that you work with a team you trust so they can walk you through both the surgery and recovery process.
If you or someone you know is affected by funnel chest, seek evaluation by specialists like Dr Harish Mithiran, an expert in chest wall deformities. At Neumark Lung & Chest Surgery Centre, our team offers comprehensive assessment, personalised treatment planning, and state-of-the-art surgical approaches tailored to individual needs.
Neumark’s thoracic surgeons specialise in the Nuss procedure, so patients receive the proper intervention. Contact Neumark to schedule a consultation for funnel chest today.

