Lung cancer is the most common type of malignant tumour in the lungs, but not all lung tumours are cancerous. Detecting tumours early, especially malignant ones, increases the chances of successful treatment. Across the world, lung cancer is a major cause of cancer-related deaths. Lung tumours in Singapore are no exception.
A lung tumour is a growth of cells within the lung tissue. Unlike temporary lung infections or inflammatory nodules, a tumour is a persistent mass that can be benign (non-cancerous) or malignant (cancerous). Benign tumours grow slowly and don’t spread, while malignant tumours can invade nearby tissues and metastasise to other parts of the body. The difference between these two is key as it determines treatment and prognosis.

Types of Lung Tumours
Lung cancer tumours can be classified along multiple lines. Firstly, there are primary lung cancers, named so because they form in the lungs. These include non-small cell lung cancer (NSCLC), the most common type, and small cell lung cancer (SCLC), which is more aggressive. Secondly, there are metastatic lung tumours which originate from other organs, such as the breast, colon, kidney or skin (melanoma), that have spread to the lungs.

Causes and Risk Factors
Lung tumours develop from a mix of lifestyle, environmental and genetic influences. Smoking is the most significant cause of malignant lung tumours, with second-hand smoke also increasing the risk. This is because harmful chemicals from tobacco damage lung cells over time, creating conditions that promote the growth of abnormal cells.
Environmental and workplace exposures, such as asbestos, radon gas and industrial chemicals, can injure lung tissue and trigger tumour formation. This risk is higher for individuals in certain industries or those residing in areas with poor air quality.
Chronic lung diseases like COPD, pulmonary fibrosis and tuberculosis can scar and weaken lung tissue, making abnormal growth more likely.
Genetics also play a role. A family history of lung cancer, certain inherited syndromes, ageing and reduced lung health can all increase susceptibility. When genetic risks combine with long-term exposure to carcinogens, the chance of developing a lung tumour and the speed at which it progresses can rise significantly. If any of the prior factors are present in your life, it is worth considering getting a scan for lung cancer.

Lung Tumour Symptoms
The symptoms of a lung tumour can be varied and depend on the size, location, and whether it has spread. Some tumours, especially in the early stages, do not show any symptoms and are found only during routine health checks or imaging for unrelated issues.
If symptoms do arise, they may include a persistent cough that does not go away, coughing up blood, shortness of breath, or chest pain that worsens with deep breathing or coughing. Other possible signs are wheezing, hoarseness, unexplained weight loss, fatigue and recurrent chest infections.
Many of these symptoms can be caused by other lung conditions and are often overlooked. However, any persistent or unusual change in breathing, especially in people with known risk factors such as smoking or chronic lung disease, should be evaluated by a healthcare professional. Early recognition and medical assessment can significantly impact treatment outcomes.

Diagnosis
Diagnosis begins with a thorough medical history and physical examination. Imaging is essential, starting with chest X-rays, followed by more sensitive scans such as low-dose CT and PET-CT to detect and characterise the lung lesions.
If a suspicious mass is found, a tissue sample is required to confirm if it is cancerous. This can be achieved through a bronchoscopy, a CT-guided needle biopsy, or a surgical biopsy. The diagnosis is confirmed by examining the tissue under a microscope. For confirmed lung cancer tumours, molecular testing may be done to determine eligibility for targeted therapies.

Staging and Classification
The TNM staging system is a method for describing the stage of malignancy in a patient’s body. The system assesses tumour size (T), lymph node involvement (N) and spread to other organs (M). Staging evaluates the extent of the tumour and whether it has spread from the lung to different parts of the body, including the lining of the lung and distant organs. This helps determine how far the cancer has spread and guides treatment decisions. Importantly, early-stage tumours confined to the lung generally have better outcomes than advanced-stage disease.

Treatment Options for Lung Tumours
At Neumark Lung & Chest Surgery Centre, if a benign lung tumour appears suspicious, is large, or shows pre-cancerous changes, our thoracic surgeon may recommend resection to confirm the diagnosis and prevent the cancer from progressing. We offer advanced minimally invasive options:
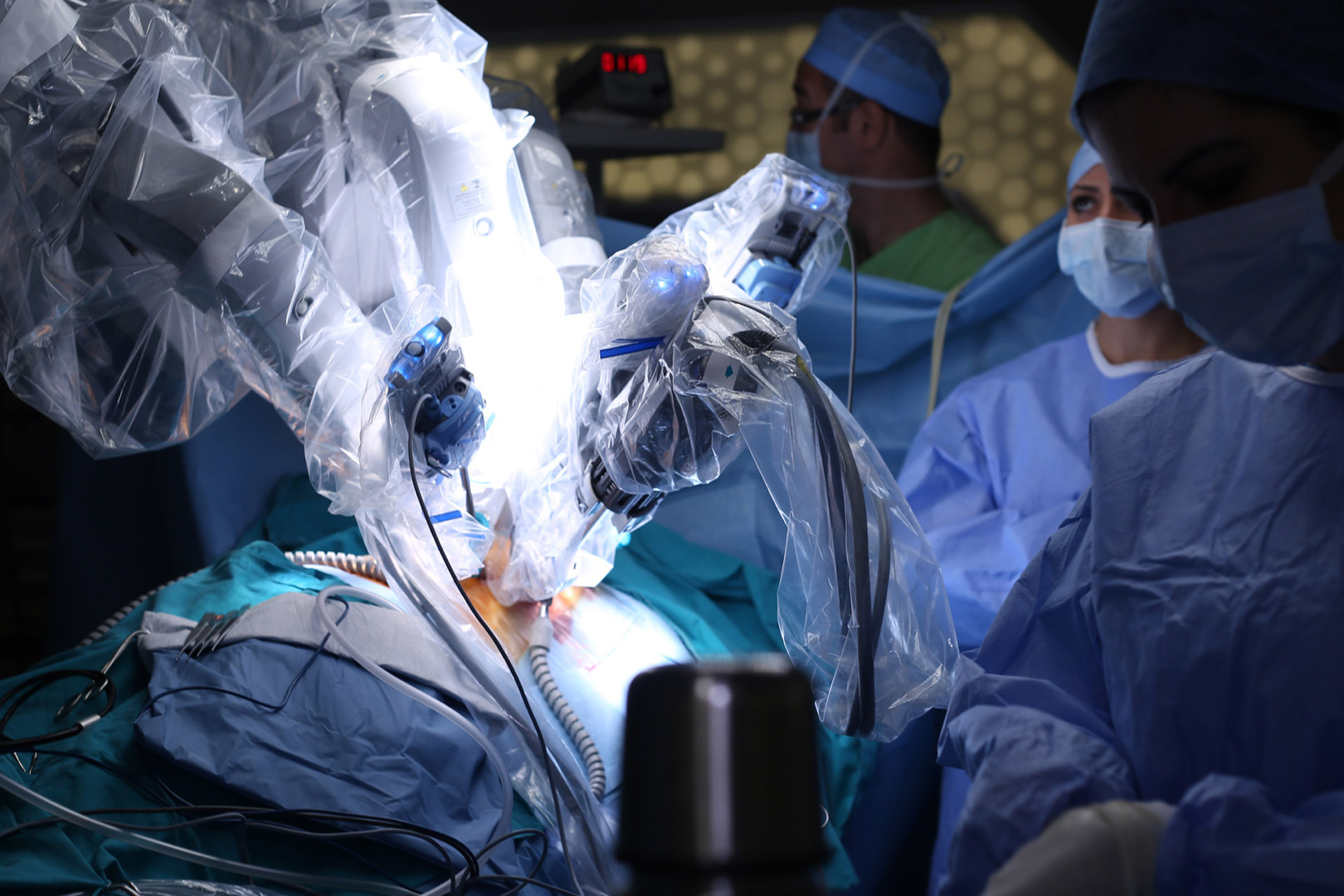
- Robotic Thoracic Surgery (RATS) with the Da Vinci system for precise, surgeon-controlled movements.
- Uniportal Video-Assisted Thoracoscopic Surgery (U-VATS), a single-incision approach that removes pulmonary nodules with minimal trauma and helps patients recover faster.
Both RATS and U-VATS are advanced, minimally invasive options that facilitate better recovery times and shorter hospital stays without compromising surgical outcomes. These highly precise options have revolutionised lung tumour assessments by making node removal or biopsies safer and more efficient.
Radiation therapy, including stereotactic body radiation therapy (SBRT), is used when surgery is not suitable. Chemotherapy, targeted therapy and immunotherapy are used in more advanced disease, sometimes in combination with surgery or radiation.
Patients are advised to avoid exposure to smoke at the very least during treatment and recovery.
Prognosis and Survival Rates
Prognosis for lung tumours depends on tumour type, stage and patient health. Early-stage lung cancer tumours removed surgically can have 5-year survival rates of 80-90%, especially before lymph node involvement. Benign tumours have an excellent prognosis and often require no further treatment beyond surveillance after removal.
Prevention and Screening
The best prevention is to avoid tobacco altogether. For smokers, quitting significantly reduces risk over time. Reducing exposure to known carcinogens and maintaining good lung health through exercise and vaccinations also helps, and regular screening programs further increase the chances of early detection for lung tumours in Singapore.
Detecting lung cancer early is key to improving survival rates and treatment outcomes. Low-dose CT screening in high-risk groups, such as those 50-80 years old with significant smoking history, can detect lung tumours early in the chest when treatment is most effective.

When to See a Specialist
Seek specialist advice if you have persistent lung tumour symptoms, unexplained respiratory changes or abnormal scan results. Multidisciplinary care at a centre like Neumark Lung & Chest Surgery Centre means you’ll receive coordinated expert evaluation from thoracic surgeons, oncologists and respiratory physicians.
If you have concerns about a lung tumour or have been advised to have further testing, contact Neumark Lung & Chest Surgery Centre today. Our team provides expert diagnosis, advanced lung tumour removal techniques and compassionate care to help you breathe easier and live well.