If a specialist suspects you have lung cancer, they will likely suggest you undergo a lung cancer biopsy. While this may sound alarming, this is a routine test that can quickly get your specialist and you a firm diagnosis.
Neumark Lung & Chest Surgery Centre offers a full range of minimally invasive biopsy techniques and coordinates your imaging, respiratory medicine and thoracic surgery, so you know what to expect at every step.
What Is a Lung Cancer Biopsy?
A lung cancer biopsy takes a small sample from a nodule, mass, lymph node or pleural fluid for microscopic review. Where indicated, the laboratory also performs biomarker testing to identify genetic alterations and PD-L1 status that can guide targeted therapy and immunotherapy. Getting enough tissue for an accurate diagnosis and a full biomarker panel without disrupting lung function is key. A good sample clarifies what the lesion is, how active it appears and which drugs or surgery will help.
Biopsy methods include imaging-guided needle sampling, bronchoscopy, and keyhole surgical biopsy if other routes are unsuitable or inconclusive. If a standard biopsy cannot be done, sputum cytology may be considered.
While imaging can suggest cancer, a biopsy is needed for a definitive diagnosis and determining the next steps.
Symptoms and Red Flags
Many lung nodules are found by chance during health screenings or scans performed for other reasons. Symptoms that require assessment include a persistent cough, coughing blood, unexplained weight loss, chest pain, breathlessness, recurrent chest infections and hoarseness that doesn’t settle. Seek urgent care if you cough up a lot of blood, develop sudden shortness of breath or have chest pain that worsens with breathing.

Causes and Risk Factors
Lung cancer develops when cells lining the airways or alveoli change and grow abnormally. Tobacco smoke is the most substantial risk factor, including second-hand exposure. Other recognised risks include a family history of lung cancer, exposure to radon or workplace carcinogens, prior chest radiation, chronic lung disease, and increasing age. In Singapore, a significant proportion of people with lung cancer have never smoked. That’s why scans and accurate diagnoses matter for everyone, not just smokers.
Diagnosis
The diagnostic pathway usually starts with a chest X-ray, followed by a contrast CT scan to characterise any abnormality. PET-CT can highlight metabolically active areas and help target the safest biopsy site. If results are unclear, further tests such as thoracoscopy, additional scans or a repeat lung biopsy may be needed for confirmation and staging.
At Neumark, we coordinate investigations so you don’t repeat tests. The aim is to choose the least invasive approach that answers the clinical question on the first attempt.

Lung Cancer Biopsy Options in Singapore
No single technique suits everyone. The position and size of the lesion, its proximity to a bronchus or the chest wall and whether lymph nodes are involved all shape the plan. Biopsy methods differ in invasiveness, anaesthesia requirements, recovery time, and suitability for specific tumour sites. Our specialists at Neumark work with you to select the option most likely to yield a diagnosis at the lowest risk.
Bronchoscopic Biopsy and EBUS
Bronchoscopy uses a thin, flexible scope passed through the mouth under light sedation or general anaesthesia, and the throat is numbed for comfort. For central tumours and enlarged lymph nodes, endobronchial ultrasound (EBUS) uses an ultrasound probe at the scope tip to sample nodes and tumours in real time. This helps with staging by allowing access to mediastinal nodes without a skin incision.
Benefits of this procedure include no skin puncture and a low risk of pneumothorax. The main limitation is that there may be tiny peripheral nodules far from the airway. Most people go home the same day after a bronchoscopic biopsy. A sore throat or mild cough usually settles within 24 to 48 hours. Cancer seeding from bronchoscopy is extremely rare.
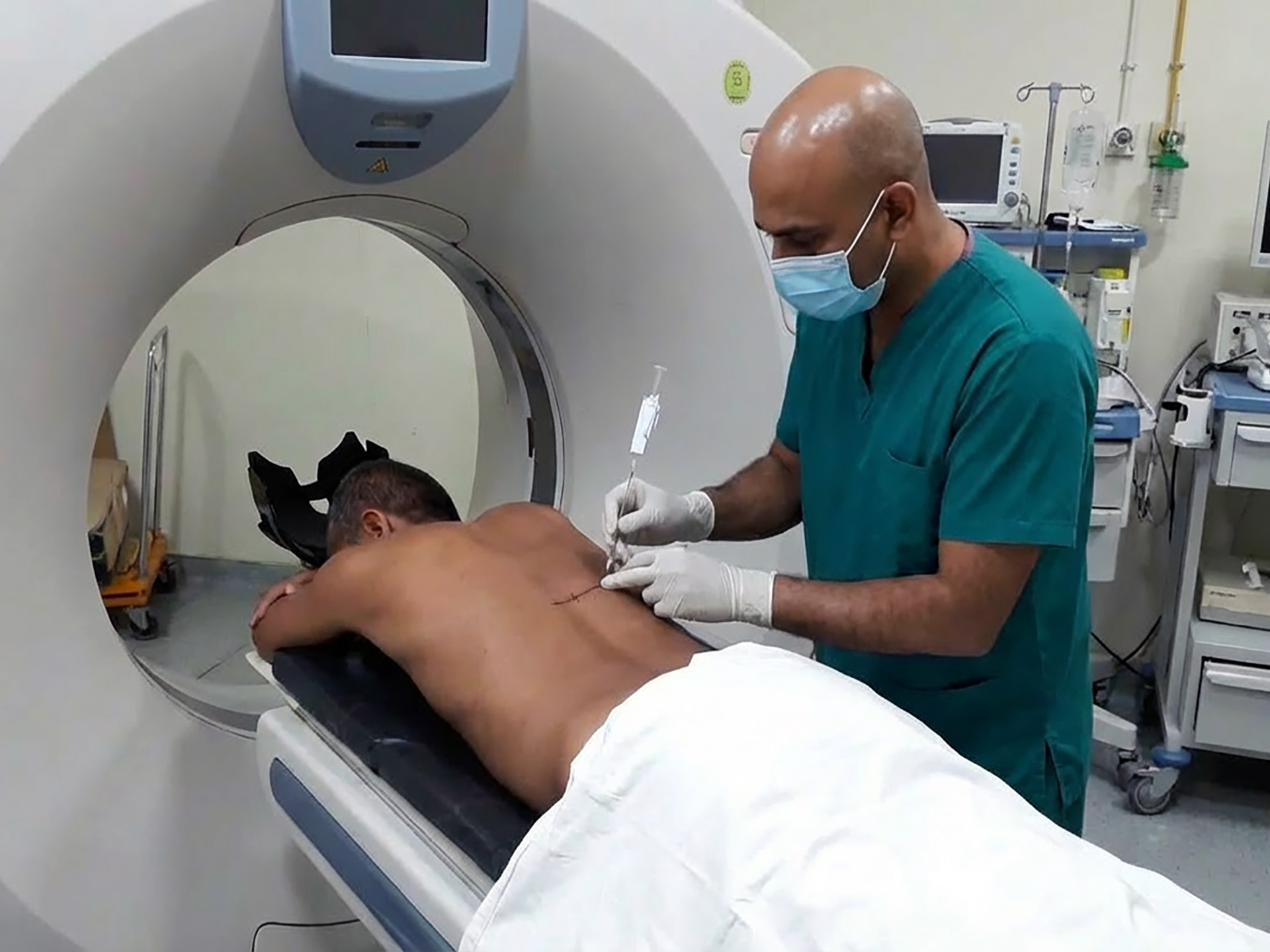
CT-Guided Needle Biopsy
For nodules near the chest wall, a radiologist can perform a CT-guided needle biopsy, also known as a transthoracic needle biopsy. After a local anaesthetic, a thin needle is advanced through the chest wall into the target while CT images guide each step. If cells are aspirated, it’s a fine needle biopsy for lung cancer. If a small tissue core is taken, it’s a core needle biopsy suited to histology and molecular testing.
This approach is highly accurate for accessible nodules and often provides sufficient tissue for gene mutation analysis in a single sitting. The main risks are pneumothorax and bleeding, so you will be observed for a few hours with post-procedure imaging. Most people still go home the same day. Needle-track seeding in the lung is extremely rare, and the benefit of early, precise sampling outweighs the theoretical risk.
VATS, U-VATS and RATS biopsy
When a lesion is small, deep, or otherwise inaccessible by other methods, a keyhole surgical biopsy can provide a definitive diagnosis. Video Assisted Thoracoscopic Surgery (VATS) uses two or three small ports between the ribs under general anaesthesia. Uniportal-VATS uses a single small incision.
Robotic Assisted Thoracic Surgery (RATS) offers the same access with finer instrument control. In each approach, the surgeon uses special instruments to obtain tissue and can remove a wedge of lung that includes the nodule. If a frozen section confirms cancer and you have consented before the operation, the procedure can proceed to a larger resection in the same sitting. These methods have a high diagnostic yield but require general anaesthesia and a short hospital stay. Still, recovery is faster than an open surgery. Most people can walk the same day and return to light activity within one to two weeks.
Pleural Fluid Analysis and Biopsy
If fluid collects around the lung, testing that fluid and, if needed, taking a pleural biopsy can confirm the cause. This condition, called a pleural effusion, requires attention. Thoracentesis uses a thin needle to remove fluid for analysis. A chest tube may be placed to drain larger volumes or manage complications. VATS thoracoscopy can obtain pleural biopsies and drain fluid in the same sitting, helping diagnose and relieve breathlessness.
Blood Tests and Liquid Biopsy
Liquid biopsy looks for tumour DNA and circulating tumour cells in a blood sample. It’s a non-invasive way to detect cancer biomarkers and can provide useful molecular information. It may help with risk assessment and post-treatment monitoring, but it does not replace tissue when a visible lesion needs characterisation.

Safety and Staging
For lung lesions, the risk of needle track seeding is very low. Bronchoscopic biopsies avoid the chest wall and carry an even lower risk. The main dangers are pneumothorax, bleeding and the small risks of anaesthesia. Imaging and biopsy also stage disease by assessing lymph nodes and distant organs, which directly guide treatment.
Treatment Pathways and What Happens after a Biopsy
A biopsy informs staging and treatment. Pathology confirms the presence of cancer and describes its features. Once histology and, where appropriate, the molecular profile and PD-L1 status are available, your oncologist and surgeon discuss options.
Early-stage disease may be treated with VATS or RATS surgery, sometimes with lymph node sampling. Others may be suitable for targeted therapy, immunotherapy, chemoradiotherapy, or a combination, depending on factors such as stage, tumour type, and patient fitness. Staging scans assess the spread to the other lung or distant organs and guide treatment. If the result is benign, options include observation or removal if symptoms persist or uncertainty remains.

Recovery and Follow-Up
Most bronchoscopic and CT-guided biopsies are day procedures. Plan to rest with light activity and avoid flying for a short period if advised. Most people return to desk work within one to two days and to gentle exercise when comfortable. After VATS, U-VATS, or RATS biopsy, expect a hospital stay of 1 to 3 nights.
Histology results usually take three to five working days, with molecular tests taking longer. If an initial report is benign, your surgeon will correlate the biopsy site with the imaging and your symptoms, and advise whether a repeat sample or a short-interval CT is needed. The goal is diagnostic certainty without unnecessary procedures.
Why Choose Neumark?
Neumark specialises in minimally invasive thoracic surgery under the leadership of Dr Harish Mithiran. Our team of respiratory physicians, oncologists, interventional radiologists and pathologists runs a coordinated biopsy service that cuts delays and tailors the approach to your anatomy and goals. We focus on precision, clear communication and recovery plans that work for life in Singapore.
If you are looking for a lung cancer biopsy in Singapore, contact Neumark Lung Cancer Treatment Centre at Gleneagles Hospital or Mount Alvernia Hospital. We will discuss your options, recommend the least invasive test that answers the clinical question and guide you from results to recovery.