Lung cancer ranks as the third most prevalent cancer in Singapore, leading to more deaths than breast, colon and prostate cancers combined. Smoking is the primary cause of the majority of lung cancer deaths, highlighting the significant impact of tobacco use on lung health. For individuals with a history of smoking, even those who have quit up to 15 years ago, concerns about lung cancer are common.
The National Cancer Centre Singapore (NCCS) updated its lung cancer screening guidelines to include individuals aged 55 to 74 who have a history of smoking 30 or more pack-years and who currently smoke or who have quit smoking within the past 15 years. These individuals are eligible for low-dose CT scans to screen for lung cancer, with annual repeat screenings recommended based on their healthcare provider’s advice.

Dr Harish Mithiran, a senior consultant thoracic surgeon at Gleneagles and Mt. Alvernia Hospitals in Singapore, emphasises that “quitting smoking is the most effective measure to reduce lung cancer mortality”. However, he also highlights that “new risk factors have been discovered in the last few years which alarm lung specialists.”
Screening is no longer only recommended for those meeting the NCCS criteria but also for groups at higher risk, including Asian women who are never smokers.
Less than a decade ago, early lung cancer screening methods were not very effective, leading to many cases being detected only in the later, more critical stages of the disease. Today, low-dose CT scans could significantly impact lung cancer mortality, unlike regular chest X-rays.
Regular lung cancer screenings might be advisable based on one’s smoking history and other risk factors. However, “unlike routine screenings like mammograms or prostate exams, lung screenings aren’t yet standard for everyone”, explains Dr Mithiran, who is also the director of Neumark Lung & Chest Surgery Centre.
He expresses optimism that “targeted screening can now identify more patients at an early, treatable stage, potentially decreasing lung cancer mortality rates and survival rates to help patients live long, healthy lives.”
Individuals eligible for lung cancer screening who are concerned about radiation exposure from CT scans can be reassured. Efforts to minimise exposure mean one low-dose CT scan emits less radiation than the average annual environmental background exposure. Thanks to technological advancements, further reductions in radiation doses without compromising imaging quality.
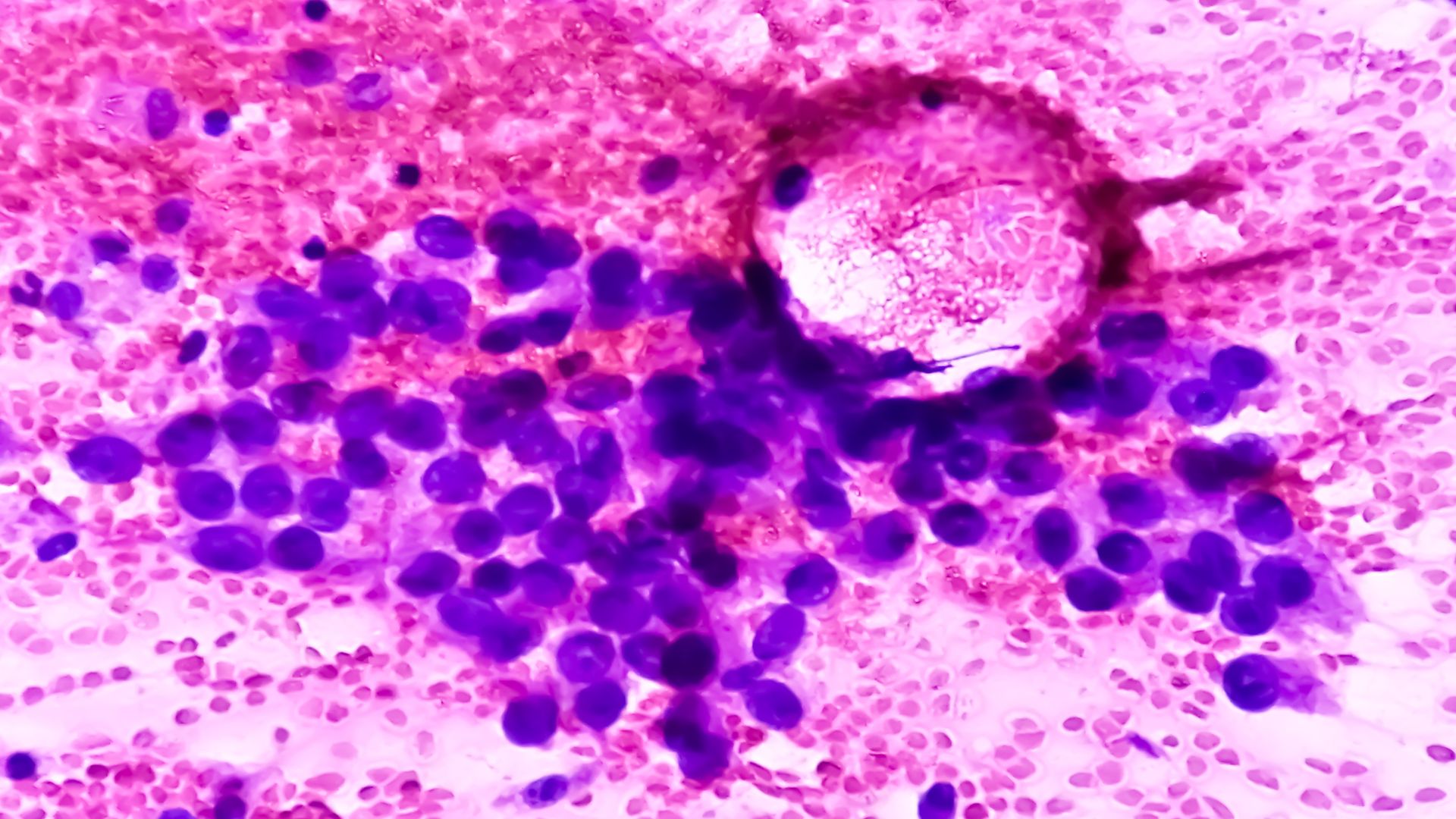
Neumark Surgery diagnoses a significant number of lung cancer patients at early stages I and II. The tumour is small, has not spread to lymph nodes or other organs, and is generally considered curable.
Eligibility for Lung Cancer Screening Beyond Standard Guidelines
Even if you don’t meet the national criteria for lung cancer screening, it might still be worth considering, especially if you have hereditary factors like a family history of the disease, are exposed to secondhand smoke or carcinogens, or have pre-existing lung conditions such as COPD or interstitial lung disease, and exposure to secondhand smoke, as well as new genetic mutations seen in this generation.
These elements can significantly increase the risk of developing lung cancer, highlighting the importance of considering personal and environmental factors in assessing your risk for developing this disease.
“Even if you don’t meet the criteria but are still concerned about lung cancer, you should consult with your primary care doctor or schedule a consultation at Neumark’s early prevention screening centre”, says Dr Mithiran.
While most private insurance providers follow specific NCCS recommendations, lung cancer screening is often available under most insurance plans. The significant challenge with CT scans is their high sensitivity. They can detect small nodules, often considered inconsequential or background noise. The vast majority of nodules will not be cancerous.
“When nodules are large enough to need further examination, our specialised thoracic team assesses those that require closer inspection, distinguishing between benign conditions and those needing intervention.”
Reasons Lung Cancer Detection Trails Other Cancer Types
Lung cancer diagnosis often lags behind other cancers because many patients don’t show symptoms until the disease has progressed to a more advanced stage. This delay in onset means that lung cancer is frequently diagnosed at a later stage, where treatment options are more limited and less effective compared to cancers detected earlier through screening programs like those for breast cancer.
Early-stage lung cancer often presents no symptoms, making regular discussions with a lung specialist crucial if you experience persistent chest pain, cough, shortness of breath, hoarseness, coughing up blood, or frequent bouts of bronchitis or pneumonia. These symptoms, especially when persistent, may indicate advanced lung cancer.
At Neumark Surgery, our multidisciplinary team includes thoracic surgeons, chest radiologists, smoking cessation specialists, and other trained members who coordinate care. The team offers personalised lung risk assessments and discusses the benefits and potential downsides of screening for each patient. Patients identified with lung nodules are advised to undergo further evaluations.
Informed Decision Process Can Be Reassuring

Neumark’s Early Screening Programme provides personalised consultations. Typically, the costs of lung cancer screening are covered by insurers. For more information or to schedule a lung screening or consultation, call Neumark Surgery at +65 6908 2145 or WhatsApp at +65 9726 2485.

