Malignant Neoplasm of the Lung Explained
A malignant neoplasm of the lung is another term for lung cancer. Like lung cancer, not all lung neoplasms are cancerous. Benign tumours, such as hamartomas, bronchial adenomas, and papillomas, are non-cancerous and often require only monitoring. However, malignant neoplasms are aggressive and need to be treated promptly.
It’s a common and serious disease, but outcomes are better when detected early and managed by a specialist team, including chest physicians, with access to modern imaging, molecular testing and advanced thoracic surgery.
An accurate cancer diagnosis is crucial as it guides treatment and can have a significant emotional impact on patients and their families. Specialist centres provide advanced care for malignant lung neoplasms.
Common Types of Lung Cancer
Most lung cancers are classified as non-small cell lung cancer or small cell carcinoma, with non-small cell lung cancer being the more common type. Non-small cell lung cancer includes subtypes such as adenocarcinoma, squamous-cell carcinoma, and large-cell carcinoma, while small-cell carcinoma is more aggressive and tends to spread rapidly.
Lung Neoplasm Symptoms
Some people have no symptoms of lung neoplasms, and a tumour may be found incidentally on a scan. In such cases, detecting a lung nodule often requires further investigation to distinguish between benign and malignant causes.
Others develop symptoms such as a persistent cough, coughing up blood, shortness of breath, chest pain, wheeze, hoarseness, recurrent chest infections, fatigue or unexplained weight loss. These are typical lung cancer symptoms, but they can be mistaken for other respiratory illnesses, making early detection challenging.
Malignant Lung Neoplasm Risk Factors
Smoking is the most substantial risk factor for a malignant neoplasm of the lung. The risk decreases after quitting, but does not disappear completely. Efforts to quit smoking are crucial for reducing the risk of lung cancer and improving overall lung health.
The other causes and risk factors for lung cancer include exposure to hazardous chemicals such as asbestos, radon, diesel fumes and air pollution. These factors contribute to developing lung cancer by causing genetic damage that leads to the mutation and proliferation of airway cells into malignant tumours, thereby increasing the risk of developing lung cancer. Family history, previous chest radiation and certain genetic changes can also increase risk. Chronic lung diseases such as COPD or pulmonary fibrosis can make the lungs more vulnerable.
The prevalence of lung cancer cases is significant in Singapore, as it is the third most prevalent type of cancer for both men and women.

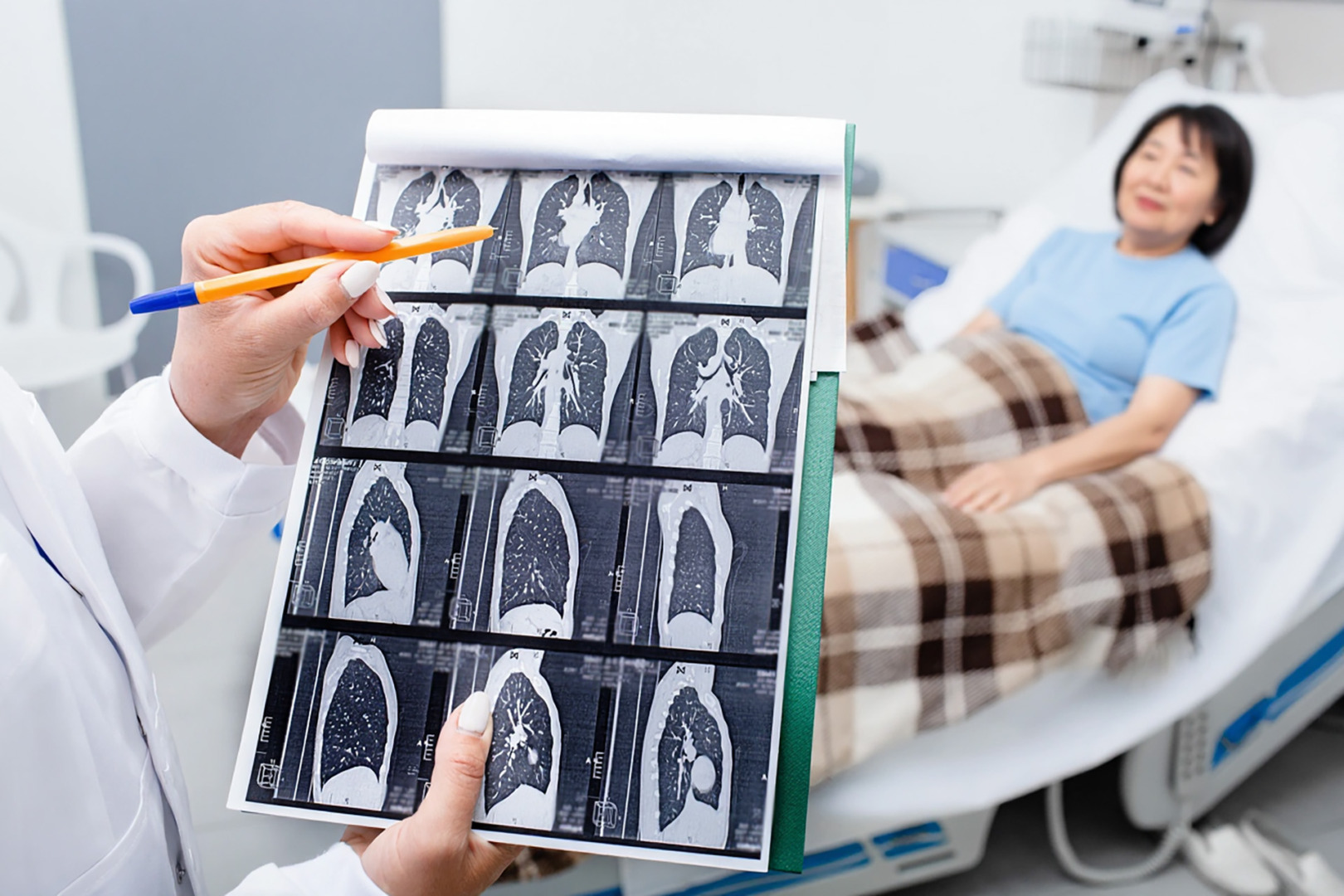
Lung Cancer Diagnosis and Staging
Diagnosis starts with a clinical assessment and imaging. A chest X-ray can raise suspicion, but a CT scan offers detailed information on tumour size, shape and location. PET CT helps to assess metabolic activity and identify the spread to other organs. If pleural fluid is present, ultrasound can guide drainage and sampling.
A diagnosis of a malignant lung neoplasm requires tissue. These biopsy procedures target lung tissue to confirm the diagnosis of lung cancer. This is done via bronchoscopy, CT-guided needle biopsy or, if necessary, a surgical biopsy.
Pathologists confirm the diagnosis and may perform molecular testing to identify mutations targeted by specific drugs. Knowing the type of lung cancer, non-small cell or small cell, is essential to guide treatment decisions.
Staging looks at the primary tumour, the involvement of nearby lymph nodes, and distant spread. Cancer spread is evaluated by determining whether lung cancer has spread to nearby lymph nodes or distant organs such as the liver. This assessment helps identify how lung cancer spreads and the extent of metastasis, informing treatment choices and prognosis.
Localised disease is more amenable to surgery, while advanced disease often requires systemic therapy. For a secondary malignant neoplasm of the lung, staging is adapted to the primary cancer, focusing on both lung involvement and disease elsewhere.

Treatment Options for Lung Neoplasms
Treatment is individualised and may include surgery, radiation therapy, chemotherapy, targeted therapy, immunotherapy and palliative care, depending on the patient’s prognosis and needs. Radiation therapy plays a key role in treating lung cancer, either before or after surgery, and can also be used to relieve symptoms in advanced cases. The goal is to control or remove the tumour, reduce symptoms, and preserve the quality of life.
When surgery or radiation therapy is used, additional treatment may be needed to target any remaining cancer cells and prevent recurrence. Immunotherapy works by activating the immune system to identify and kill cancer cells, offering new options for patients with advanced or hard-to-treat lung cancers. Palliative care is also essential, focusing on symptom management and the quality of life for patients at any stage.

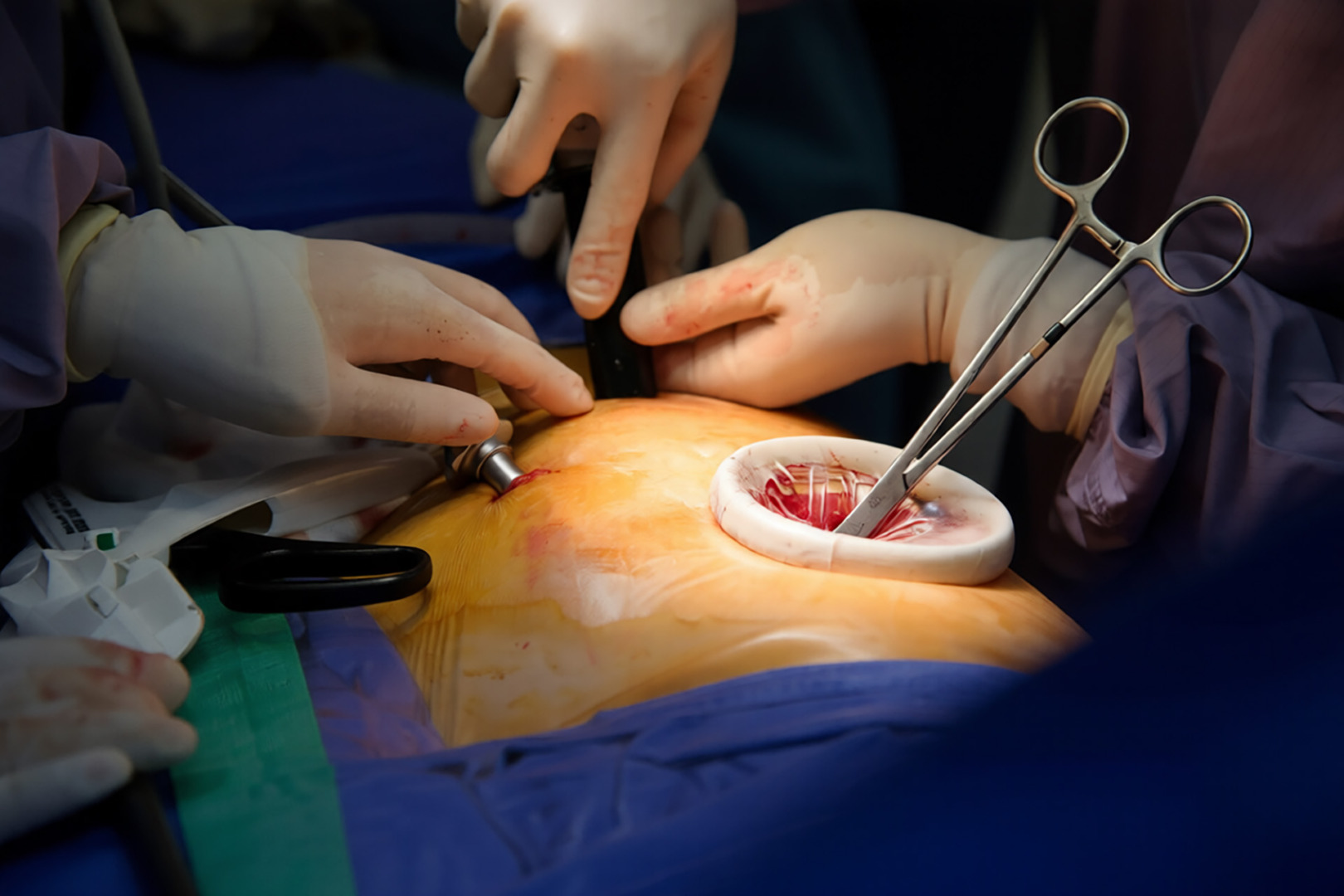
Minimally Invasive Thoracic Surgery
Modern thoracic surgery has moved towards minimally invasive techniques that limit trauma while achieving precise results. Surgery offers the best chance for a cure for the early stages of lung cancers and can provide durable control in select cases.
Surgery is often indicated for localised lung tumours, including both primary lung tumours and some secondary tumours that have metastasised to the lungs. Some of the advanced methods used at Neumark Lung & Chest Surgery Centre include:
- Video-Assisted Thoracoscopic Surgery (VATS), which uses small incisions and a camera to access the chest
- Robotic-Assisted Thoracic Surgery (RATS), which provides three-dimensional vision and articulated instruments for fine dissection, is especially useful in deep or complex resections
- Uniportal VATS, which achieves similar results through a single small incision
The surgeon can perform wedge resection, segmentectomy or lobectomy and remove lymph nodes for accurate staging. In some cases where lung tumours are localised but extensive, a pneumonectomy may be performed, which involves removing an entire lung to achieve complete cancer removal. These approaches reduce pain and recovery time compared to open surgery while maintaining high standards of cancer clearance.
When Surgery Is Not The First Line
If the disease has spread extensively or the patient is not a surgical candidate, non-surgical treatment is preferred. Systemic therapies include chemotherapy, targeted agents based on tumour mutations, and immunotherapy. Radiotherapy targets local disease or eases symptoms such as pain or airway obstruction. In some cases, treatment starts with drugs, and if there is a good response, surgery may follow to leverage on that success.
A secondary malignant neoplasm of the lung may still be resectable if the number of lung metastases is small and the primary cancer is under control. Selected patients with limited spread, such as those with a few colorectal lung metastases, may benefit from minimally invasive lung surgery after multidisciplinary review.

Symptoms and Complications
If pleural fluid accumulates, it may need to be drained, and in some cases, a pleurodesis is done to prevent recurrence. Narrowed airways may require intervention to restore airflow. In advanced disease, surgery still has a role in managing complications that are not responding to medical or radiotherapy treatment.
Follow-Up and Recurrence Prevention
Follow-up after treatment includes physical examination and scans. The aim is to detect recurrence early, manage side effects and support recovery. Lifestyle changes such as quitting smoking, staying active within safe limits and keeping vaccinations up to date are helpful for long-term recovery.
The risk of recurrence depends on tumour stage, biology, and completeness of initial treatment. Thorough surgery with proper lymph node assessment, together with adjuvant therapy when needed, reduces this risk. If a new lesion is found, the team re-evaluates and plans the next step, which may include repeat minimally invasive surgery, targeted therapy, or radiotherapy.

Lung Cancer Screening and Early Detection
Many lung cancers develop silently. Early-stage lung cancer often has no symptoms and is usually only found through medical imaging, so early detection is key to better outcomes. Low-dose CT screening for high-risk individuals, such as older smokers or those who recently quit, can help detect tumours at an earlier stage. This increases the chances of successful treatment and may allow for less extensive surgery. Screening is not for everyone, so it’s worth discussing the personal risks and potential benefits with a specialist.
Multidisciplinary Care
Outcomes are best when specialists work together. A multidisciplinary team, including thoracic surgeons, medical and radiation oncologists, respiratory physicians, radiologists, pathologists, and specialist nurses, ensures each case receives the appropriate treatment.
Neumark Lung Cancer Treatment Centre in Singapore has extensive experience in VATS, RATS, and U-VATS, and can tailor surgery to the tumour’s location and the patient’s health while preserving function. Our collaborative approach is built into the care pathways at Gleneagles Hospital and Mount Alvernia Hospital. Consult a specialist at Neumark today.

