If you or a family member has been told there’s fluid around the lungs, it helps to know precisely what that means. This could be pulmonary oedema vs pleural effusion, two different problems that both involve fluid and breathlessness, yet develop in other places, have various causes, and follow different treatment paths.
At Neumark Lung & Chest Surgery Centre, led by senior consultant thoracic surgeon Dr Harish Mithiran, we coordinate imaging, specialist assessment and, when indicated, procedures for pulmonary oedemas and pleural effusions at Gleneagles Hospital on Napier Road and Mount Alvernia Hospital on Thomson Road.
What Are Pulmonary Conditions?
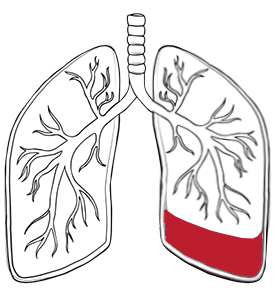
Pulmonary conditions like pulmonary oedema and pleural effusion are serious health issues that can affect your ability to breathe comfortably. Pulmonary oedema occurs when excess fluid accumulates in the air sacs (alveoli), making it difficult for oxygen to pass into the bloodstream. This causes shortness of breath and difficulty breathing, which can be scary and needs prompt attention. Pleural effusion, on the other hand, is when fluid collects outside the lungs in the pleural space and can also cause breathing difficulties.
Understanding the underlying causes, such as congestive heart failure, high altitude pulmonary oedema and noncardiogenic pulmonary oedema, is key to management and treatment. Knowing the signs and when to seek help can make all the difference in outcomes for these pulmonary conditions.
What’s the Difference and Why It Matters
In pulmonary oedema, fluid accumulates in the lungs’ air sacs as it leaks from the lung’s vascular network, which transports blood. This fluid interferes with gas exchange, leading to lower oxygen levels and more difficult breathing. Pulmonary congestion refers to the accumulation of fluid within the lung tissue, further impairing oxygen exchange and worsening breathing difficulties. Most cases are due to the heart not pumping efficiently, but non-cardiac triggers also exist.
In pleural effusion, fluid builds up between the lung and the chest wall. As a result, the lung is externally compressed and cannot fully expand. Pleural fluid can be watery, inflammatory or infected, and the cause ranges from heart failure and liver disease to pneumonia, cancer and tuberculosis. Because the fluid sits in different places in these two conditions, investigations and treatment differ.
Understanding pulmonary oedema vs pleural effusion early makes a difference and avoids delays:
| Feature | Pleural Effusion | Pulmonary Oedema |
| Location | Fluid collects in the pleural space between the lungs and the chest wall. | Fluid collects in the lungs, in the air sacs (alveoli), and in the tissue. |
| Causes | Exudative: pneumonia, cancer, tuberculosis, pulmonary embolism. Transudative: heart failure, kidney disease, liver failure, cirrhosis. | Often caused by heart failure, kidney failure, or severe hypertension. |
| Symptoms | Shortness of breath, chest pain, and a cough that can be dry or productive (brings up mucus). | Shortness of breath, especially when lying down, a feeling of suffocation, and a cough that produces frothy, blood-tinged sputum. |
| Mechanism | Fluid can compress the lungs, making it hard to breathe. | Fluid interferes with gas exchange in the air sacs, lowering oxygen levels. |
| Common complication | Can occur as a consequence of pulmonary oedema as fluid leaks from the lung into the pleural space. | Can lead to pleural effusion. |
Types of Pulmonary Oedema
Pulmonary oedema can be classified into two main types: cardiogenic and noncardiogenic.
Cardiogenic pulmonary oedema is most common in heart failure, where the heart is unable to pump blood well, leading to increased pressure in the lung’s blood vessels and fluid leaking into the air sacs.
Noncardiogenic pulmonary oedema is due to factors unrelated to heart function. These include acute respiratory distress syndrome (ARDS), lung injury, severe infections or exposure to high altitudes, known as high altitude pulmonary oedema. In this form, low oxygen levels or direct lung tissue injury can lead to fluid accumulation. Identifying the underlying cause of pulmonary oedema is key as treatment and prevention strategies depend on addressing the specific trigger, whether it is heart failure, lung injury or high altitude exposure.
Symptoms and Red Flags
Both conditions can cause shortness of breath.
Pulmonary oedema often causes breathlessness that worsens when lying flat, a feeling of suffocation at night, and a cough that may produce frothy, sometimes blood-tinged sputum. People may notice ankle swelling, rapid weight gain due to fluid retention, and a fast heartbeat.
Chronic pulmonary oedema symptoms can include episodes of breathlessness while sleeping, causing individuals to wake up gasping for air.
Pleural effusion tends to cause chest tightness or a dull ache on one side, a dry or productive cough and breathlessness that may ease a little when sitting upright. If the pleural fluid becomes infected, there may be fever, chills and pleuritic pain that sharpens with deep breaths.
Seek urgent care if you develop severe breathlessness at rest, blue lips, confusion, high fever or chest pain that is new or worsening. These are warning signs that require immediate assessment in Singapore’s emergency services.
Causes and Risk Factors
When comparing causes of pulmonary oedema vs pleural effusion, think inside the lungs versus outside the lungs. Pulmonary oedema is most often heart-related. Cardiogenic pulmonary oedema is due to heart failure, where the heart can’t pump blood well, and fluid accumulates in the lungs. Additionally, left-sided heart failure, acute coronary syndromes or severe high blood pressure increase pressure in the lung vessels and fluid seeps into the air sacs.
Non-cardiac causes include acute respiratory distress, severe infections, high altitude exposure, especially with rapid ascents, kidney failure and some medications or toxins. Chronic pulmonary oedema and long-term pulmonary oedema develop gradually with underlying conditions and cause ongoing symptoms like episodic breathlessness and peripheral swelling.
Pleural effusion occurs when fluid production in the pleural space exceeds the body’s ability to clear it. Transudative effusions occur with heart failure, cirrhosis or nephrotic syndrome. Exudative effusions reflect inflammation or blockage and include pneumonia, pulmonary embolism, malignancy like lung cancer or metastatic disease and tuberculosis, which is still an essential diagnosis in the region. Smoking, prior lung disease, recent surgery and history of cancer all increase the risk of both conditions.

Complications of Pulmonary Oedema
If pulmonary oedema is not treated early, it can lead to serious and life-threatening complications. The most severe cases can progress to respiratory failure, where the lungs can no longer supply enough oxygen to the body, or even cause cardiac arrest.
Pulmonary oedema can also increase the risk of developing pleural effusion, pneumonia and acute respiratory distress syndrome (ARDS). In some cases, abnormal fluid accumulation can promote the formation of a blood clot in the lungs, leading to a pulmonary embolism — a medical emergency. Since symptoms of pulmonary oedema can escalate quickly, seek immediate medical attention if you have severe shortness of breath, chest pain or other warning signs.
Diagnosis of Pleural Effusion in Singapore
Diagnosing pulmonary oedema involves a thorough clinical assessment, listening to lung sounds, and ordering diagnostic tests such as imaging and blood tests to confirm the presence of fluid in the lungs and the underlying cause.
A review of medical history is key to guiding diagnosis and underlying conditions. Auscultation reveals diffuse crackles for pulmonary oedema, dullness to percussion, and absent breath sounds for a pleural effusion. In Singapore, a typical workup is quick, often within the same day in private care.
Whether it be pulmonary oedema vs pleural effusion, an X-ray is the first step for both. In pulmonary oedema, the film may show a bat-wing pattern of central haze, Kerley B lines (short horizontal lines) suggesting interstitial fluid, an enlarged heart, and fluid in the fissures. These findings indicate excess fluid in the lung’s alveoli, which can impair oxygen intake and cause breathlessness.

In a pleural effusion, the costophrenic angle, the short indentation where the diaphragm meets the ribs, is blunted, with a fluid meniscus and reduced visibility of the diaphragm on the affected side. Your specialist will be able to explain the imaging results to you. Pleural effusion is indicated by a homogeneous opacity with blunting of the costophrenic angles and a meniscus sign. Since patients often ask about pulmonary oedema vs pleural effusion on X-ray, it’s helpful to emphasise that radiological patterns point in different directions, though overlap can occur.
An ultrasound is more sensitive than a chest X-ray for detecting small amounts of pleural fluid. Bedside ultrasounds add clarity to your condition. In pulmonary oedema, the presence of vertical artefacts called B-lines on ultrasound indicates the presence of interstitial fluid. In pleural effusion, an ultrasound confirms the presence of free or loculated pleural fluid and guides safe drainage. When required, a CT scan characterises underlying lung disease, loculations, pleural thickening, or masses. Blood tests assess infection, kidney and liver function, cardiac markers and inflammatory indices. Blood oxygen levels are also monitored to determine the impact of fluid accumulation on oxygen intake.
If pleural effusion is confirmed, a diagnostic thoracentesis removes a small sample of fluid for analysis. In suspected malignancy, a pleural biopsy may be recommended. Neumark coordinates this so results go back to your consultant quickly. Many patients undergo imaging at Gleneagles Hospital or Mount Alvernia Hospital and proceed to drainage or further tests the same day if clinically indicated. The prognosis of pulmonary oedema depends on the underlying cause and the speed of intervention, with prompt treatment leading to better outcomes.

Treatment Options for the Conditions
Management depends on the cause of the effusion and the severity of breathlessness. Here are some options for pulmonary oedema and pleural effusion.
Medical Therapy
- Heart failure-related effusion: diuretics and guideline-directed cardiac medication.
- Malignant effusion: oncologic therapy tailored to tumour type, which may include chemotherapy, targeted therapy or immunotherapy. Palliative radiotherapy can help with local pain or obstruction, but does not routinely clear pleural fluid.
- Parapneumonic effusion: antibiotics based on culture and local practice.
Drainage and Procedures
- Diagnostic and therapeutic thoracentesis: ultrasound-guided needle drainage to relieve symptoms and analyse fluid.
- Chest tube thoracostomy: for larger, recurrent or infected collections, or when continuous drainage is required. In selected empyema, intrapleural tPA and DNase can help break down loculations.
Surgical Options
- Video-Assisted Thoracic Surgery (VATS): preferred minimally invasive approach to break septations, evacuate pus, perform decortication for trapped lungs, and deliver talc pleurodesis when recurrent effusion is expected. Most patients mobilise early with shorter hospital stays than with open surgery.
- Indwelling pleural catheter (IPC): for recurrent malignant effusion, enabling outpatient drainage and symptom control. It can be combined with talc pleurodesis if the lung expands.
- Open thoracotomy: reserved for very dense adhesions, late organised empyema or when minimally invasive surgery is not safe or effective.

Prevention of Pulmonary Oedema
Preventing pulmonary oedema starts with managing underlying health conditions that increase the risk of fluid accumulation in the lungs. This includes managing heart disease, kidney disease, high blood pressure and avoiding known triggers like high altitudes when possible.
Adopting a healthy lifestyle, such as a balanced diet, regular exercise and stress management, can reduce the risk of developing pulmonary oedema. Working with your doctor to manage coronary artery disease and high blood pressure is key to reducing your risk of pulmonary oedema and long-term lung health.
Recovery and Follow-Up
Recovery from pulmonary oedema depends on the underlying cause. Many patients feel better within days once fluid shifts and oxygenation improve. Long-term care focuses on heart health, medication adherence, weight monitoring, and regular review with a cardiologist or primary care provider. Patients with long-term pulmonary oedema or chronic pulmonary oedema require ongoing monitoring and management to prevent recurrence.
After drainage of a pleural effusion, discomfort at the needle site usually resolves within a day. If VATS is performed, most patients start walking the next day, do breathing exercises with physiotherapy, and have drains removed within a few days once the lung is expanded.
Follow-ups include a wound review, a chest X-ray or ultrasound to confirm resolution, and a plan to prevent recurrence. This may involve optimising heart or liver function, completing antibiotics, pursuing oncologic therapy or vaccination and smoking cessation support.

Why Neumark?
Neumark Lung & Chest Surgery Centre combines specialist thoracic expertise with a practical patient-centred pathway. The team coordinates imaging, consultation and procedures across Gleneagles Hospital and Mount Alvernia Hospital so you don’t have to wait. When surgery is needed, we favour minimally invasive approaches to shorten hospital stays and speed recovery. When surgery is not the answer, we will focus on medical treatment with the right specialists.

If you are unsure what condition you have or have been advised to consider drainage or surgery, we can review your scans and plan the next steps together. For clear answers and a tailored plan, contact Neumark Lung & Chest Surgery Centre to see Dr Harish Mithiran at Gleneagles Hospital or Mount Alvernia Hospital.