Stage 3 lung cancer treatment generally involves a combination of different therapies, such as chemotherapy, radiotherapy, and in some cases, surgery. Stage 3 lung cancer indicates that the cancer has gotten to a point where it’s no longer a localised problem but has spread to other parts of the lung, and potentially beyond.
At Neumark Lung & Chest Surgery Centre in Singapore, a team of specialists led by senior consultant thoracic surgeon Dr Harish Mithiran manages Stage 3 lung cancer cases at Gleneagles or Mount Alvernia hospitals.
The Basics of Lung Cancer
Lung cancer starts when abnormal cells in the lungs begin to grow out of control, forming a tumour that can interfere with breathing and possibly spread to other parts of the body. It is one of the most common cancers and a leading cause of cancer deaths in Singapore.
There are basically two types of lung cancer:
- Non-small cell lung cancer (NSCLC), which accounts for about 90% of all lung cancer cases, includes subtypes such as squamous cell carcinoma, adenocarcinoma and large cell carcinoma.
- Small cell lung cancer (SCLC), which makes up the remaining 10%, tends to grow and spread more quickly.
Early detection, through lung cancer screening, can make a significant difference. Treating lung cancer at an early stage obviously gives patients the best chance at an optimal outcome. To diagnose lung cancer, thoracic surgeons use CT scans to spot any abnormal growths, often followed up by a biopsy to confirm the diagnosis and determine the stage. Unfortunately, most lung cancers are diagnosed at an advanced stage because the symptoms can be subtle.
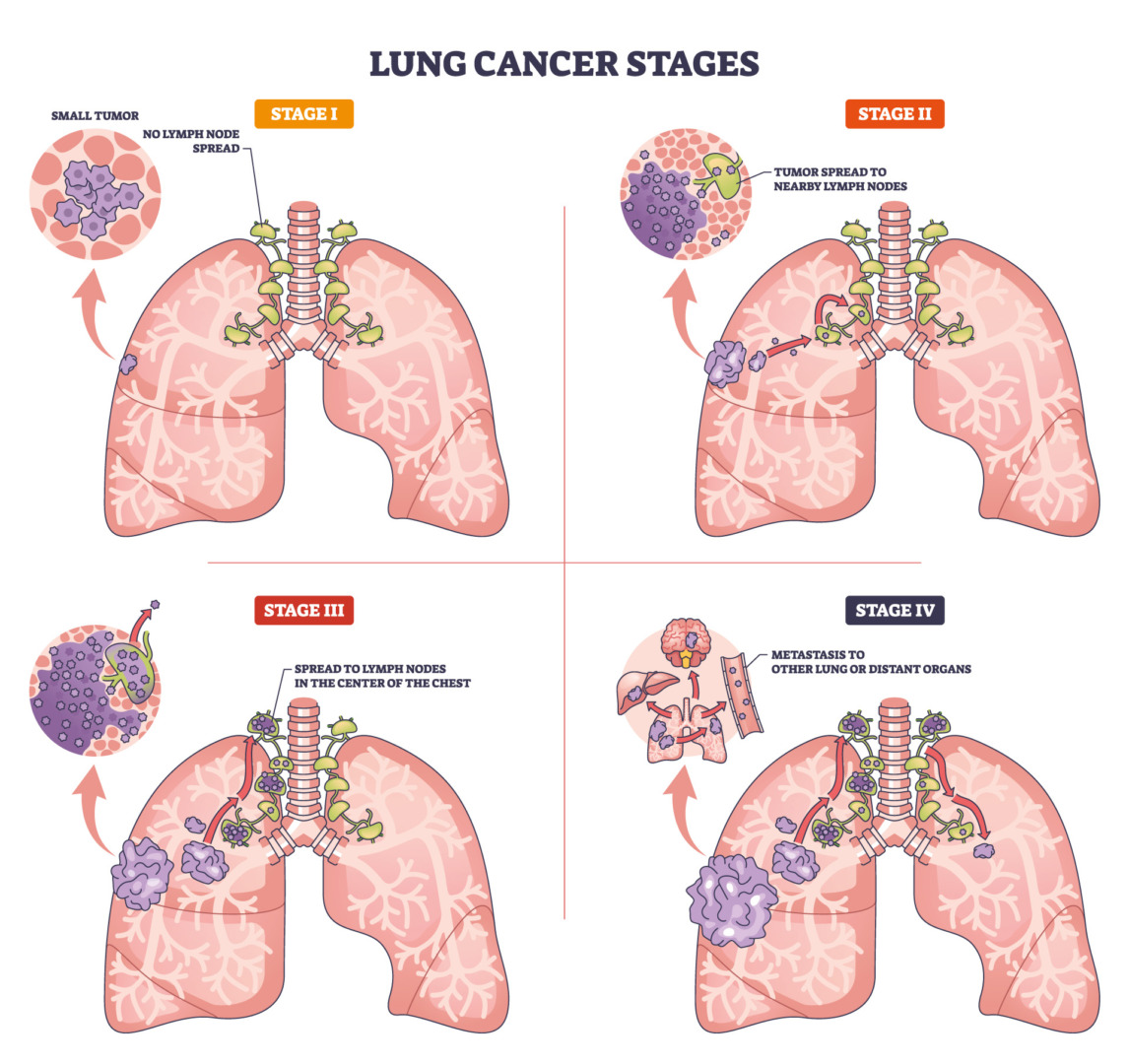
Staging of Lung Cancer
To describe lung cancer in detail, lung specialists use the TNM staging system. This system is primarily used to stage non-small cell lung cancer (NSCLC) and provides information on the primary tumour, lymph nodes and metastasis.
- T (Tumour): Describes the size and extent of the primary tumour and how far it’s grown into nearby tissue or structures like the chest wall, diaphragm, heart or major blood vessels.
- N (Nodes): Indicates whether cancer cells are present in nearby lymph nodes and which groups of nodes are affected.
- M (Metastasis): This indicates whether the cancer has spread to distant organs; in all Stage 3 cases, M is 0 (M0), as there’s no distant spread.
The table below gives the specific characteristics of Stage 3 lung cancer:
| Stage | Where the cancer is | What this usually means for treatment |
| Stage 3A NSCLC | The tumour is in one lung and may have grown into nearby structures such as the chest wall or diaphragm. Cancer has spread to lymph nodes on the same side of the chest, often including mediastinal nodes, but has not spread to distant organs. | This is a locally advanced disease. Some patients may still be eligible for surgery after initial chemotherapy or chemoradiotherapy. |
| Stage 3B NSCLC | The tumour may be similar in size to Stage 3A or larger and can invade vital structures such as the heart, major blood vessels, or the oesophagus. In this case, the cancer has spread to lymph nodes in the centre of the chest on the opposite side or above the collarbone, but there is still no spread to distant organs. | These cancers are generally not suitable for surgery at the outset. Treatment usually focuses on chemoradiotherapy and immunotherapy. |
| Stage 3C NSCLC | The tumour is large and/or has invaded several critical structures in the chest. Lymph node involvement can be extensive (on one or both sides of the chest), but there is still no distant spread. | This is an advanced, locally aggressive disease and is rarely suitable for surgery. A multimodal treatment approach is usually recommended. |
Stage 3 Lung Cancer Symptoms and Red Flags
Knowing what Stage 3 lung cancer symptoms are like can help with spotting symptoms early and starting treatment quicker. These symptoms can have a significant impact on daily life and often prompt people to seek care from a lung specialist.
Common symptoms include:
- A persistent cough that worsens or changes
- Coughing up blood or blood-stained phlegm
- Finding it more challenging to breathe or having wheezing
- Chest pain that gets worse when you take a deep breath or cough
- Getting chest infections over and over, which don’t clear up
- Hoarseness or changes to your voice if the cancer affects the nerve to the voice box
- Having trouble swallowing if the tumour is squashing the oesophagus
- Unexplained weight loss, feeling tired, or a loss of appetite
- Swelling of the face, neck or upper body if the tumour blocks a major blood vessel
- Having fluid build-up in the chest, such as a pleural effusion
If you experience any of the following, see a lung specialist as soon as possible: coughing up a lot of blood, getting suddenly very short of breath, or chest pain; getting some swelling of the face and neck; or noticing new confusion, weakness, or a massive headache. These symptoms usually need urgent attention.

Causes & Risk Factors
In Singapore and generally across the world, cigarette smoking remains the most significant cause of lung cancer. The chemicals in cigarette smoke damage lung tissue and can cause cancerous cells to form. The risk increases the more you smoke and the longer you’ve been smoking, although it’s worth noting that lots of people with the disease have never smoked.
In Singapore and Asia, nearly half of lung cancer cases occur in non-smokers, suggesting that unique genetic or environmental factors are involved. Potential risk factors include second-hand smoke, air pollution, industrial fumes (e.g., asbestos), radon, prior chest radiotherapy, diesel exhaust, arsenic in drinking water, and family history. However, having risk factors does not guarantee cancer, and many Stage 3 patients have no apparent cause.

Early Detection & Screening
Patients with a high risk of developing lung cancer, such as heavy smokers between the ages of 50 and 80, may be offered low-dose CT screening to check for lung cancer at an earlier stage. Screening isn’t suitable for everyone, but it can find tumours before symptoms appear, which is often a much better time to start treatment.
Screening criteria usually involve individuals who have smoked for 30 or more pack years and are still smoking or have quit less than 15 years ago. Pack years are calculated by multiplying the number of cigarette packs you smoked each day by the number of years you smoked.
If you’ve smoked heavily for a long time or have other risk factors, you can talk to your doctor about whether screening is proper for you. Screening programmes are available through Neumark Lung & Chest Surgery Centre, which will arrange the necessary scans and follow-up care if an abnormality is detected.

Diagnosis and Staging in Singapore
A typical assessment involves a detailed consultation, a good physical examination, a high-resolution chest CT scan and usually a PET CT scan to see how far the disease has spread, and if it’s gone any further than just the lung itself, lung function tests to see how well you can breathe, some blood tests to check on your overall health, and a biopsy to confirm the diagnosis and what type of cancer it is.
The biopsy might be performed using a thin, flexible tube with a camera (bronchoscopy) to reach the tumour, a needle biopsy in which a needle is inserted through the chest wall under CT guidance, or a surgical biopsy if the other methods aren’t suitable. During these procedures, tissue samples are taken from the abnormal areas and sent to the lab to confirm the presence of lung cancer.
The pathologists will then review the tissue samples to confirm the cancer type and perform molecular testing to identify the gene mutations and protein markers involved, which can help guide targeted treatments and immunotherapy.
Comprehensive Staging Tests for Stage 3 Lung Cancer
Once Stage 3 lung cancer has spread to lymph nodes or nearby structures, having a thorough staging process is essential to know what the best treatment approach is. Further tests usually include:
Endobronchial Ultrasound (EBUS)
This tool lets our surgeon feed a thin tube down your windpipe and use ultrasound to guide a needle into the middle of your chest to get a closer look at the mediastinal lymph nodes.
Mediastinoscopy
This surgery is performed while you are entirely under anaesthesia, which lets doctors take a closer look at and sample the lymph nodes in the mediastinum when the EBUS results aren’t clear enough, or they need a bit more tissue.
Video-Assisted Thoracoscopic Surgery (VATS) for Staging
An operation that uses a camera and tiny incisions to get at the lymph nodes in your chest and get some more samples.
Brain MRI Scan
To rule out any cancer that might have metastasised to your brain.
PET CT Scan
This advanced imaging pinpoints the location of disease activity within the body. It is critical to distinguish whether enlarged lymph nodes are due to a malignancy or an inflammatory infection.
Bone Scan
This diagnostic imaging evaluates the bones for metastatic lesions. It is clinically indicated for patients presenting with bone pain or abnormal biochemical markers that raise concern for skeletal disease.
These tests determine if the cancer is operable or too advanced for surgery. They also check if a bone scan necessitates shifting to chemotherapy and other control treatments, or if apparent Stage 3 is actually Stage 4, having spread elsewhere.
At Neumark, Dr Harish personally goes through all your test results and scans. He works closely with a team of medical oncologists, radiation oncologists, respiratory specialists, and radiologists, all based at Gleneagles and Mount Alvernia hospitals, to get a complete picture and develop the best treatment plan for your Stage 3 lung cancer.

Stage 3 Lung Cancer Treatment Options
Stage 3 lung cancer treatment options are more complex than earlier stages and usually require a combination of therapies. The specific treatment plan depends on the sub-stage (3A, 3B or 3C), the size and location of the tumour, which lymph nodes are involved, whether the tumour can be surgically removed, your lung function and overall health, and the results of molecular testing.
For most patients with Stage 3 lung cancer, the primary treatment approach is chemoradiotherapy, which combines chemotherapy and radiotherapy given together to control the tumour in the chest. In carefully selected cases of Stage 3A disease, lung cancer surgery may be considered as part of a multimodal treatment plan, usually after initial chemotherapy or chemoradiotherapy to shrink the tumour.
When chemotherapy is given before surgery to reduce tumour size, this is known as neoadjuvant chemotherapy. Immunotherapy has become an essential addition to treatment and may be given after chemoradiotherapy or in combination with chemotherapy.
Role of Surgery in Stage 3 Lung Cancer
Unlike Stages 1 and 2 lung cancer, where surgery is typically the first treatment, the role of surgery in Stage 3 lung cancer is more selective.

Resectable Stage 3A
Some patients with Stage 3A disease may be candidates for surgery, particularly those with limited N2 lymph node involvement (cancer in mediastinal lymph nodes on the same side as the primary tumour). These patients usually receive neoadjuvant chemotherapy first. If the tumour responds well and the patient remains fit, surgery may then be performed to remove the tumour and affected lymph nodes.
Surgery After Induction Therapy
When surgery is planned for Stage 3A lung cancer, it typically follows 3 to 4 cycles of chemotherapy or a course of chemoradiotherapy. Repeat staging scans are performed to confirm the tumour has not progressed and is removable. The surgical procedure is usually a lobectomy, removing the cancerous lobe along with an extensive lymph node dissection. In some cases, more extensive resection may be needed if the tumour involves the chest wall, diaphragm or other nearby structures.
Minimally Invasive Techniques
Dr Harish specialises in minimally invasive thoracic surgery, including Video-Assisted Thoracic Surgery (VATS), Uniportal VATS (U-VATS), and Robot-Assisted Thoracic Surgery (RATS). In selected Stage 3A patients whose tumours have responded well to induction therapy and whose anatomy is favourable, these approaches can produce better outcomes. These approaches use small incisions between the ribs and specialised instruments to remove the tumour and lymph nodes with less tissue trauma than traditional open surgery. Minimally invasive surgery can reduce postoperative pain, shorten hospital stays, and speed recovery, though its feasibility depends on the specific characteristics of each case.
When Open Surgery Is Necessary
In many Stage 3 cases, particularly when there is invasion of the chest wall, major blood vessels or other structures, or when there are extensive adhesions from previous treatment, open surgery through a larger thoracotomy incision may be required. This allows the surgeon better access and control to safely remove the tumour and manage any complications during the procedure.
Stage 3B and 3C Disease
Surgery is rarely appropriate for Stage 3B lung cancer or 3C because these tumours are either too large, involve critical structures that cannot be safely removed, or have spread to lymph nodes on the opposite side of the chest or above the collarbone. For these patients, treatment options focus on chemoradiotherapy and systemic therapies rather than surgical resection.
Chemoradiotherapy for Stage 3 Lung Cancer
For most patients with Stage 3 lung cancer, concurrent chemoradiotherapy is usually the primary treatment approach. This means chemotherapy and radiotherapy are given at the same time, which is more effective than giving them one after the other. For patients who cannot handle the concurrent treatment, a sequence of chemotherapy followed by radiotherapy may be an option.
Chemotherapy
Chemotherapy is typically platinum-based and is made up of drugs like cisplatin or carboplatin combined with other agents such as etoposide, pemetrexed or a taxane. The specific chemotherapy regimen is chosen based on the cancer type, your kidney and heart function, and your general health. Chemotherapy is usually given through an IV drip and works by targeting fast-growing cancer cells all over the body.
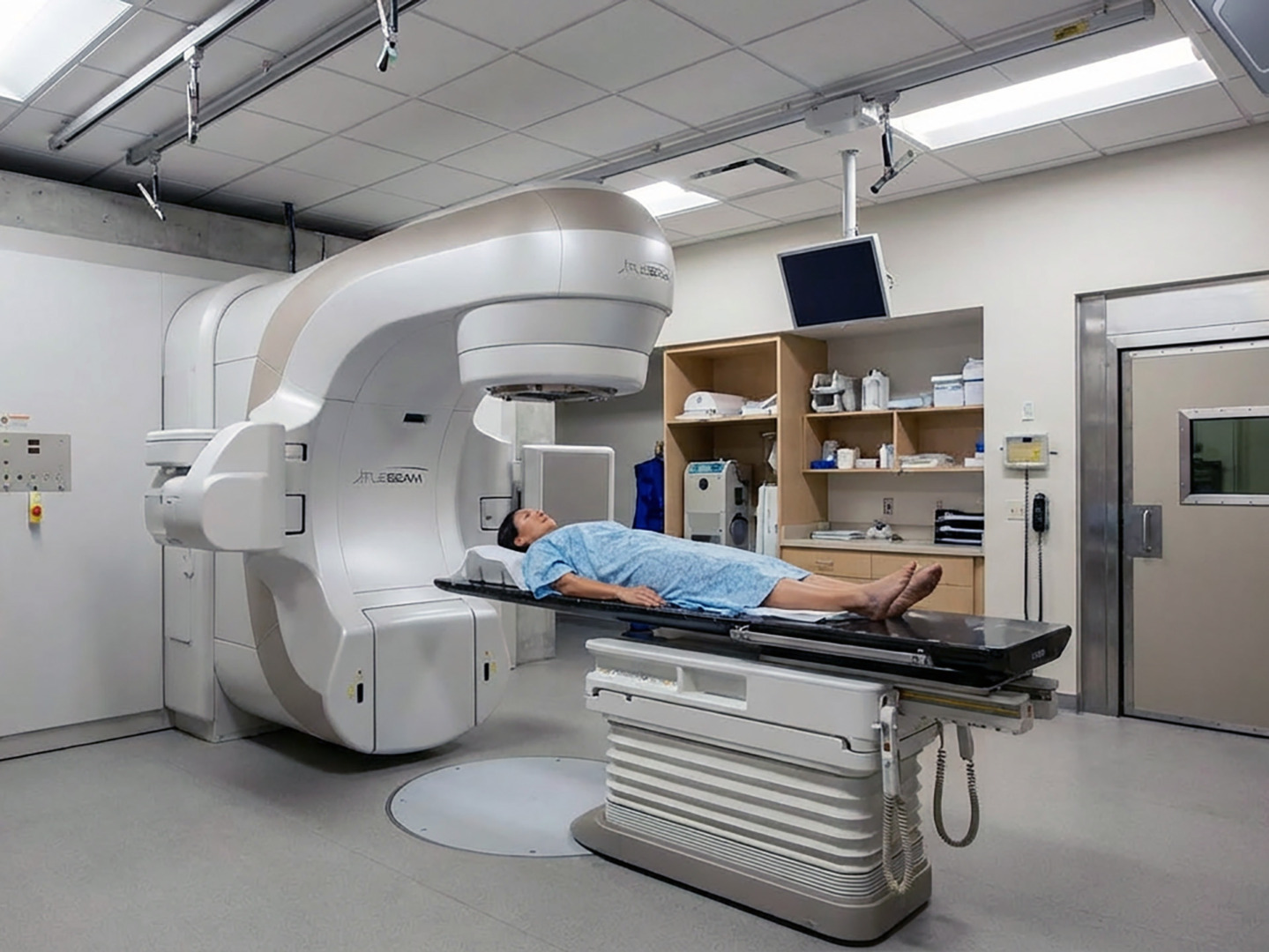
Radiotherapy
External beam radiotherapy delivers high-energy beams to the tumour and affected lymph nodes from outside the body. Treatment plans are carefully worked out using CT scans and sometimes PET scans to get an exact map of where the cancer is and make sure the radiation targets the tumour while keeping the healthy lung tissue, heart, spinal cord and oesophagus untouched as much as possible. Radiotherapy targets explicitly and wipes out lung cancer cells, and is often used as a first line of treatment for specific stages of non-small cell lung cancer (NSCLC) and small cell lung cancer (SCLC). Modern techniques such as VMAT and IMRT can reduce radiation doses to normal organs and improve treatment precision. Radiotherapy is generally given 5 days a week for 5 or 7 weeks, each session lasting only a few minutes.
Side effects of Chemoradiotherapy
Chemoradiotherapy can cause a range of side effects, including fatigue, nausea, loss of appetite, inflammation of the oesophagus (oesophagitis) that makes swallowing tricky or painful, radiation pneumonitis (inflammation of the lung tissue), skin changes in the treated area, a cough, and low blood counts that can increase the risk of infection or bleeding. Most of these side effects are temporary and can be managed with medication, dietary changes, and supportive care. Your medical team will keep a close eye on you throughout treatment and guide you in managing these side effects.
Durvalumab Immunotherapy After Chemoradiotherapy
If the cancer hasn’t progressed after concurrent chemoradiotherapy, consolidation immunotherapy for Stage 3 with durvalumab is now the standard of care. This immune checkpoint inhibitor is given by IV every 2 to 4 weeks for up to a year. It has been shown to significantly improve survival by activating your immune system to help fight cancer. Immunotherapy lets your immune system spot and attack any remaining cancer cells, rather than just going after the tumour itself. Biomarker testing checks for specific mutations, such as EGFR, to help guide targeted or immunotherapy in lung cancer treatment.
Systemic Therapies and Biomarker Testing
Biomarker testing examines biopsy tissue to identify specific gene changes and protein markers. This will help your specialist select the most appropriate treatment. For Stage 3 lung cancer, this is particularly important because it can help identify people who might benefit from targeted therapies.
| Biomarker / Mutation | What it is | How can it guide treatment |
| EGFR mutation | A change in the epidermal growth factor receptor (EGFR) gene that drives tumour growth. | Patients may be treated with EGFR tyrosine kinase inhibitors, which are tablets that block the abnormal EGFR protein. These can be used from the start or after chemoradiotherapy. |
| ALK, ROS1 and other rearrangements | Gene rearrangements (such as ALK or ROS1) that create abnormal fusion proteins driving cancer growth. | They are less common than EGFR mutations, but when present, targeted therapy can be very effective. |
| PD-L1 expression | A protein on the surface of cancer cells that can help them evade the immune system. | Higher PD-L1 expression often predicts better response to immunotherapy. |
Combination Immunotherapy and Chemotherapy
In some Stage 3 lung cancer treatment plans, immunotherapy and chemotherapy might be combined from the start, rather than just after chemoradiotherapy. This approach is still being refined through clinical trials, and your medical oncologist can let you know if this is an option for you.
The goal of systemic therapies in Stage 3 lung cancer is not just to control the tumour in the chest but also to get rid of any microscopic cancer cells that might have spread beyond the visible tumour, which in turn reduces the risk of cancer recurrence.
Treatment for Stage 3 Small Cell Lung Cancer
Stage 3 small-cell lung cancer (SCLC) is often referred to as limited-stage disease when it is confined to one side of the chest. Treatment typically involves combination chemotherapy with cisplatin or carboplatin and etoposide, given concurrently with radiotherapy to the chest.
After completing chemoradiotherapy, patients who have responded well to treatment may be offered prophylactic cranial irradiation (PCI) to reduce the risk of brain metastases developing later, as small-cell lung cancer has a high tendency to spread to the brain. For limited-stage small cell lung cancer (SCLC), the typical approach is concurrent chemoradiotherapy followed by prophylactic cranial irradiation.
The treatment approach and prognosis for Stage 3 SCLC differ significantly from those of non-small cell lung cancer, and your medical oncologist will discuss the specific plan for small cell disease if this is your diagnosis.
Clinical Trials and Emerging Treatments
Some patients with Stage 3 lung cancer may be eligible to participate in clinical trials testing new treatments, drug combinations, or different care sequences. These are research studies that have been carefully laid out and overseen by people who are watching out for the patient’s welfare. The idea behind them is to give people access to new therapies that aren’t yet ready for general use, and to help specialists learn more about what works in lung cancer treatment.
It’s worth keeping in mind that there’s no promise that a trial drug will be any better than what you’d get from conventional treatment. However, for a few patients, trials offer a last-resort option that can be a lifesaver when other options aren’t working satisfactorily. Neumark is situated in Gleneagles and Mount Alvernia hospitals, connecting it with the medical oncologists at these centres and giving us a better idea of which clinical trials are available in Singapore. Most importantly, they can help determine whether you’d be a good fit for a trial based on your specific type of cancer, its location, the genetic markers we can see, and your overall health.
Recovery, Follow-Up and Prognosis
The course of treatment for Stage 3 lung cancer is often lengthy, spanning several months and involving multiple treatment modalities. Recovery and follow-up are tailored to the treatments you have received.
| After Chemoradiotherapy | After Surgery for Stage 3A Lung Cancer |
| Most side effects gradually improve over the weeks and months after treatment. Fatigue may persist for several months. Inflammation of the oesophagus or lungs typically settles within a few weeks. If you proceed to immunotherapy, you will have regular infusions and monitoring for up to a year. | Most patients stay in the hospital for around 5 to 7 days. Breathing exercises and early mobilisation help reduce complications. At home, light activities can resume over several weeks, with full recovery taking 2 to 3 months. Additional chemotherapy or radiotherapy may be given after surgery, depending on the pathology results. |
Stage 3 Lung Cancer Survival Rates and Prognosis
While Stage 3 lung cancer is more advanced and challenging to treat than earlier stages, it is not necessarily a death sentence, and some patients can achieve long-term remission or even a cure with modern treatment approaches.
Stage 3 lung cancer life expectancy and survival rates vary widely depending on the substage, treatment received and individual factors. Stage 3 lung cancer life expectancy with treatment is significantly better than the Stage 3 lung cancer survival rate without treatment, which is generally very poor, as untreated lung cancer progresses rapidly.
Five-year survival for Stage 3 NSCLC varies by sub-stage. Stage 3A patients who undergo successful surgery after induction therapy may have 5-year survival rates of around 25 to 35%, while those treated with chemoradiotherapy alone typically have 5-year survival rates of around 15 to 25%. The average 5-year survival rate for Stage 3B lung cancer is 26%. The addition of immunotherapy for Stage 3 lung cancer, particularly durvalumab after chemoradiotherapy, has further improved these figures. Stage 3B and 3C have lower survival rates, generally ranging from 10 to 15% at 5 years, although individual outcomes vary considerably.
For Stage 3 small-cell lung cancer, outcomes are generally poorer because the disease is more aggressive. However, some patients achieve long-term remission with intensive chemoradiotherapy and prophylactic cranial irradiation. Remission can be durable, lasting for years, although ongoing monitoring is essential.
Long-Term Follow-Up
Follow-up after Stage 3 lung cancer treatment typically includes regular clinic visits every 3 to 6 months for the first few years, then annually, periodic CT scans to monitor for recurrence and side effects of chemotherapy, radiotherapy, targeted therapy or immunotherapy. It might also include lung function tests if you have had extensive radiotherapy or surgery, as well as ongoing support for symptom management and quality of life.
Your doctor will monitor for potential late effects of treatment, such as lung fibrosis (scarring), heart problems from radiation exposure, or long-term effects of chemotherapy. Regular surveillance is vital because recurrence is possible, and early detection of new problems enables timely intervention.
In addition to medical follow-up, ongoing lifestyle modifications such as maintaining smoking cessation, eating a balanced diet, staying physically active within your limits, and attending pulmonary rehabilitation if recommended can contribute to better long-term outcomes and quality of life.

Supportive Care and Living Well After Treatment
Pulmonary rehabilitation, a structured programme of exercise, breathing techniques, and a bit of confidence, can make a huge difference in your breathing capacity and stamina. Your professional team can help: your physiotherapist, dietitian, occupational therapist, and smoking cessation specialists all play essential roles in helping you regain strength, maintain nutrition, and reduce the risk of further lung problems. If you still smoke, quitting at any stage improves your response to treatment, reduces complications and improves overall health. Support for smoking cessation is available through Neumark and partner institutions.
Psychological and emotional support for patients and families is equally important. A diagnosis of Stage 3 lung cancer can be overwhelming, and feelings of fear, uncertainty, sadness or anger are entirely normal. Counselling, support groups, and open conversations with your medical team can help you and your loved ones navigate this arduous journey. Do not hesitate to ask for help when you need it.
Palliative care focuses on improving quality of life and managing symptoms at any stage of illness, not only at the end of life. Palliative care specialists work alongside your surgeon, medical oncologist and radiation oncologist to ensure you remain as comfortable and active as possible through your Stage 3 lung cancer treatment and beyond. This may include pain management, nutritional support, management of breathlessness, and practical assistance with daily activities.

Why Choose Neumark
Neumark Lung & Chest Surgery Centre focuses on comprehensive lung cancer care with expertise in minimally invasive thoracic surgery, including VATS, U-VATS and RATS procedures. Dr Harish Mithiran has extensive experience in complex lung resections, lymph node dissections, and managing locally advanced lung cancer. He works closely with medical oncologists, radiation oncologists, respiratory physicians and radiologists based at Gleneagles and Mount Alvernia hospitals to provide coordinated, multidisciplinary care.
Neumark also provides practical support with arranging diagnostic tests, staging investigations, liaising with insurance for pre-authorisation, and coordinating surgery, chemotherapy and radiotherapy around your work and family commitments. For patients in Singapore, working with a dedicated lung cancer treatment centre means rapid access to diagnostic imaging and biopsies, multidisciplinary teams who plan the best treatment approach, coordinated care across surgery, medical oncology and radiation oncology, and personalised follow-up and supportive care.
To discuss personalised Stage 3 lung cancer treatment and determine whether you are a candidate for surgery as part of a multimodal treatment plan, contact Neumark for a consultation with Dr Harish Mithiran.

