The mediastinum is the central compartment of the chest cavity between the lungs. It houses many vital structures, including the heart, major blood vessels, oesophagus, lymph nodes and other organs. A mass in the superior part of this space presents unique challenges that require specialist expertise and careful management.
A superior mediastinal mass is any abnormal tissue growth in the upper part of the mediastinum above the level of the heart’s upper chambers. These growths in the mediastinum can be benign cysts, enlarged lymph nodes or more concerning malignant tumours. Understanding these growths, their causes, and the available treatment options will empower you to make informed decisions about your care.
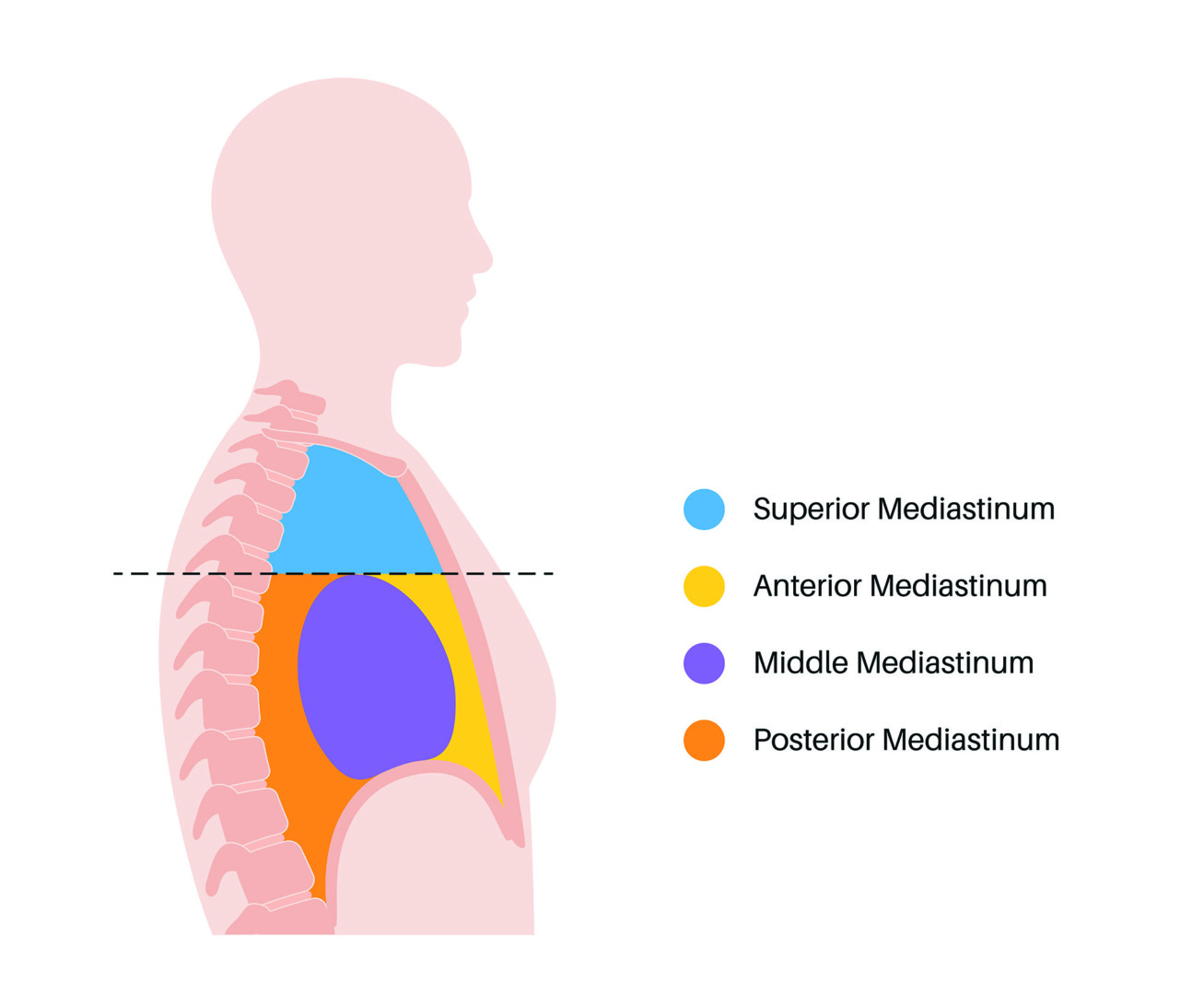
The Anatomy of Superior Mediastinal Masses
The superior mediastinum is a specific area of the mediastinum that goes from the thoracic inlet at the base of the neck down to an imaginary line drawn from the sternal angle to the 4th thoracic vertebra. This small space contains several critical structures, including the aortic arch, superior vena cava, trachea, oesophagus and many lymph nodes. When masses occur in this area, they can compress or displace these vital structures, causing adverse effects or symptoms.
The confined nature of the superior mediastinum means even small masses can cause major symptoms. Symptoms often begin early due to compression of adjacent structures. Unlike other body parts, where growths may remain unnoticed for extended periods, superior mediastinal masses typically announce themselves through their impact on surrounding structures. This anatomical fact often leads to earlier detection, benefiting treatment outcomes.
Common Causes and Types of Superior Mediastinal Masses
There are many possible causes of a superior mediastinal mass. Some are benign (non-cancerous), while others may be malignant (cancerous) and require urgent treatment. One of the more common causes is lymphoma, a type of blood cancer that begins in the lymph nodes. Hodgkin lymphoma, for instance, often shows up in this part of the chest, especially in teenagers and young adults. B-cell lymphoma is another form that can grow rapidly and cause symptoms such as fever, night sweats, and weight loss.
Another source of these masses is the thymus gland, located in the upper chest, which plays a crucial role in the immune system during childhood. The thymus usually shrinks in adults, but sometimes it can form tumours called thymomas or thymic carcinomas. These may be linked to autoimmune conditions, such as myasthenia gravis, which affects muscle strength and function.
Thyroid goitres, which are enlarged thyroid glands, can sometimes grow downward into the chest and form a mass behind the breastbone. These goitres are usually non-cancerous but can press on nearby structures and may need to be surgically removed.
Although nerve-related tumours typically appear in the back of the chest, they can occasionally be found in the upper mediastinum. These tumours grow from nerve tissue and are usually slow-growing and benign.
Some blood vessel abnormalities, such as a misshapen aortic arch or a ‘vascular ring’, may look like a mass on a scan. While these aren’t true tumours, they can still press on the trachea or oesophagus and cause symptoms like trouble breathing or swallowing.

What Are The Signs and Symptoms of a Superior Mediastinal Mass?
The symptoms of a superior mediastinal mass are often due to compression or displacement of adjacent structures within the chest. Superior vena cava syndrome is one of the most serious signs, which occurs when the mass compresses the large vein that returns blood from the upper body to the heart. Patients may experience facial swelling, particularly around the eyes, arms and upper chest. The development of prominent veins across the chest wall is a visual indicator of this compression.
Respiratory symptoms occur when the mass compresses the trachea or main bronchi. Patients may notice shortness of breath, particularly when lying flat, a chronic cough, or a feeling of chest tightness.
Some people may face difficulties swallowing if the mass compresses the oesophagus. These patients may also feel food sticking in the throat or chest, or experience difficulty swallowing both solids and liquids. Voice changes, including hoarseness, can occur if the mass affects the recurrent laryngeal nerve, which controls the function of the vocal cords.
Constitutional symptoms, such as unexplained weight loss, night sweats, and persistent fatigue, may accompany superior mediastinal masses, particularly if they stem from systemic conditions like lymphoma. Chest pain, while less common, can worsen with deep breathing or coughing.

Related Mediastinal Conditions
Diagnosis and Imaging
A chest X-ray is often the first diagnostic tool used to detect a mediastinal mass, although its findings may be inconclusive and prompt further imaging studies.
A thorough clinical assessment, including detailed history-taking and a physical examination, is the first step in evaluating a suspected superior mediastinal mass. Subsequently, imaging studies are key in characterising these masses and planning treatment approaches.
Computed tomography (CT) scanning with contrast enhancement provides detailed information about the mass’s size, location, and relationship to surrounding structures. CT images can often distinguish between different types of masses based on their appearance and enhancement patterns, which significantly alters treatment approaches. CT scans also help identify signs of invasion into adjacent structures or the presence of additional masses elsewhere in the chest.
Magnetic resonance imaging (MRI) offers superior soft tissue contrast and is particularly useful when evaluating masses near major blood vessels or when CT findings are inconclusive. The MRI image can also provide information about vascular invasion and the relationship between masses and the spinal cord or nerve roots.
Positron emission tomography (PET) scanning, often combined with computed tomography (CT), helps distinguish between benign and malignant masses by identifying areas of increased metabolic activity. This imaging is particularly useful in staging lymphomas and monitoring treatment response as seen in PET images.
Tissue diagnosis often requires biopsy procedures, which can be performed using various approaches depending on the location and characteristics of the mass. CT-guided needle biopsies are a minimally invasive option for accessible masses, while mediastinoscopy or thoracoscopic approaches may be needed for deeper or more complex lesions.

Minimally Invasive Surgical Options
Advances in minimally invasive surgery have revolutionised the management of superior mediastinal masses. These techniques offer patients shorter recovery times, reduced postoperative pain and improved cosmetic results compared to open surgery.
Video-assisted thoracoscopic surgery (VATS) is a major advancement in managing mediastinal masses. This technique uses small incisions through which the surgeon inserts a camera and special instruments to remove the mass while minimising trauma to surrounding tissues. VATS procedures result in shorter hospital stays and faster return to normal activities.
Robotic-assisted thoracic surgery (RATS) provides surgeons with greater dexterity, enhanced visualisation, and improved precision for minimally invasive surgery. The robotic platform enables complex dissections in tight spaces, making it particularly useful for the removal of superior mediastinal masses. The 3D high-definition visualisation system allows surgeons to identify and protect vital structures with unprecedented accuracy.
For some superior mediastinal masses, particularly those involving the thymus, complete removal through minimally invasive approaches has become the standard of care. These techniques allow for thorough removal while preserving important structures and minimising complications.

Recovery and Long-term Outcomes
Recovery after removal of a superior mediastinal mass varies depending on the surgical approach, the characteristics of the mass, and individual patient factors.
Minimally invasive procedures enable faster recovery, with many patients returning home within one to three days of surgery.
Pain management has evolved significantly as multimodal approaches incorporate regional anaesthesia techniques that provide excellent pain control while minimising the need for narcotic medications. Early mobilisation and pulmonary rehabilitation also help prevent complications and speed recovery.
Long-term outcomes for patients with benign superior mediastinal masses following complete surgical removal are generally excellent. For malignant masses, outcomes depend on the tumour type, stage, and the response to additional treatments, such as chemotherapy or radiation therapy.
Regular follow-up care is essential for all patients, with imaging studies and clinical assessments to monitor for any signs of recurrence. The multidisciplinary approach, involving thoracic surgeons, oncologists, and other specialists, ensures comprehensive care throughout the treatment journey.

Why Specialised Care Matters
The complexity of superior mediastinal mass management highlights the importance of seeking care from experienced thoracic surgery centres. These centres offer the expertise, technology and support services to achieve optimal outcomes.
Advanced surgical techniques, comprehensive diagnostic capabilities, and coordinated care teams deliver the best possible treatment experience to patients. At Neumark Lung & Chest Surgery Centre, we offer all three, using the latest surgical techniques with patient-centred care to achieve the best patient outcomes for those with superior mediastinal masses.
If you or a loved one has a superior mediastinal mass, don’t wait to get an expert opinion. Contact Neumark Lung & Chest Surgery Centre today to book a consultation with our thoracic surgery team. We will provide the specialist care and support you need at this difficult time and guide you through the latest treatment options.

