Thymus gland cancer is one of the rarer types of cancer. However, that does not make it any less important in understanding, especially for patients and families going through a diagnosis.
When thymus gland cancer develops, it comes in two main types: thymomas and thymic carcinomas. These cancers both originate from the epithelial cells that line the thymus gland but exhibit distinct growth patterns and require different treatment responses. Understanding these differences is key for patients to get the proper treatment.
What Is Thymus Gland Cancer?
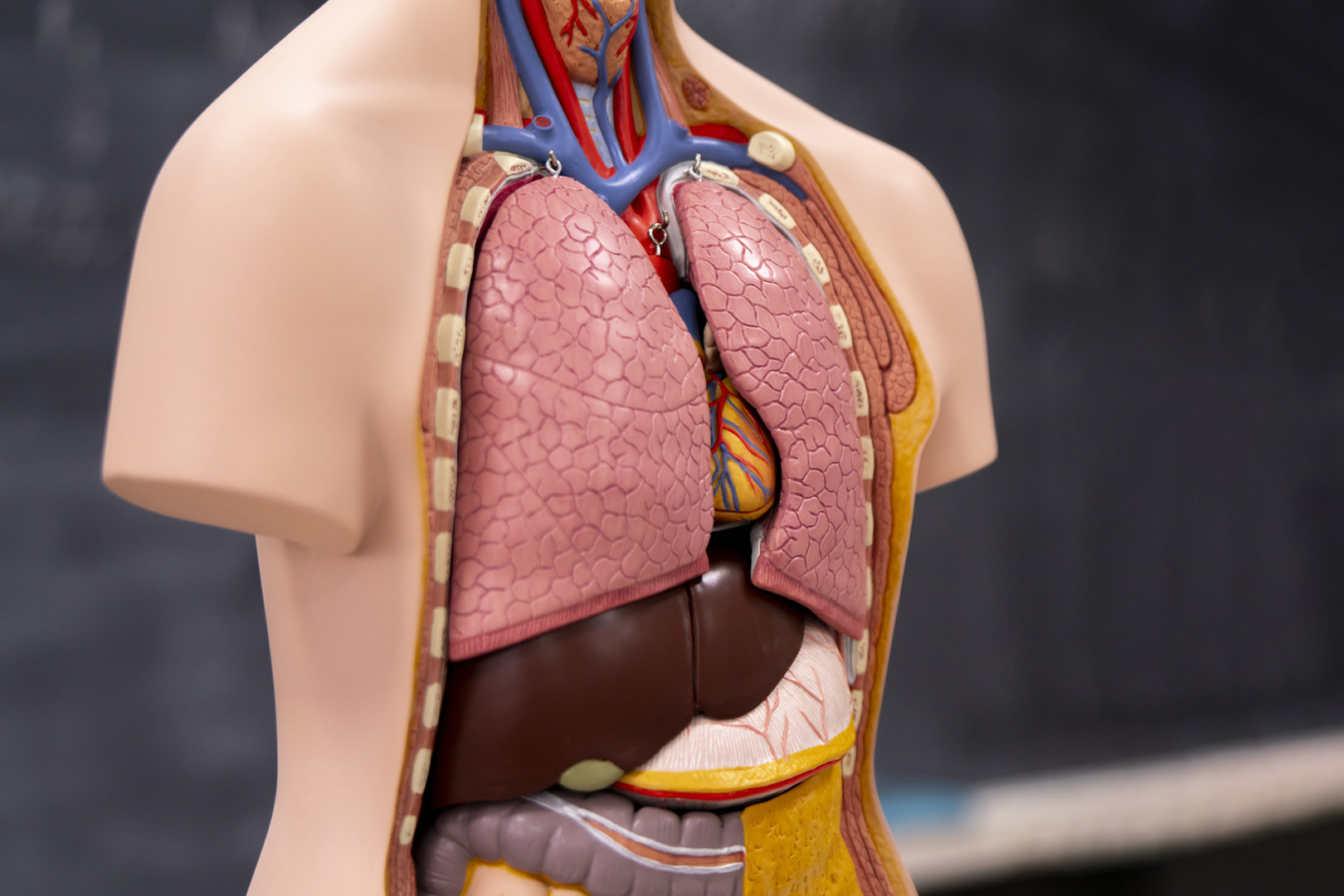
Thymus gland cancer is a type of cancer that develops in the cells that cover the outer surface of the thymus gland. This small organ, situated in the upper chest, above the heart and below the breastbone, is a component of the lymphatic system. During childhood and adolescence, the thymus produces T-lymphocytes, which mature into infection-fighting white blood cells that patrol the body for our entire lives.
The two main types of thymus gland cancer behave differently and, as such, require different treatment methods. Thymomas grow slowly and rarely spread beyond the thymus, with cancer cells that look like normal thymus tissue. Thymic carcinomas grow faster, spread more extensively, and contain cancer cells that resemble nothing like normal thymus tissue.
Thymomas typically affect individuals between 40 and 60 years old, but can occur in younger individuals as well. Thymic carcinomas account for approximately 1 in 5 thymus gland cancers and are more challenging to treat due to their aggressive nature.
What Are the Symptoms of Thymus Gland Cancer?
Many patients with thymus gland cancer have no symptoms at all. Instead, the tumour is discovered incidentally during chest imaging for another condition. When symptoms do occur, they are usually due to the tumour pressing on surrounding chest structures and can include the following:
- Persistent cough that won’t go away
- Shortness of breath
- Chest pain
- Voice hoarseness
These symptoms occur when the cancer has grown big enough to press on nearby areas in the chest. A worrying complication is superior vena cava syndrome, which occurs when the tumour compresses the large vein that carries blood to the heart. This causes swelling in the face, chest and upper neck, as well as shortness of breath and chest pain. Patients with these symptoms require urgent attention.
Thymus gland cancer is also often associated with autoimmune conditions. Up to 50% of people with thymoma develop symptoms of myasthenia gravis, a rare condition of the immune system that causes muscle weakness. Other associated conditions are red cell aplasia, hypogammaglobulinemia, pernicious anaemia, systemic lupus erythematosus, and rheumatoid arthritis.

What Is the Survival Rate for Thymus Gland Cancer?
Thymus gland cancer survival rates vary greatly depending on many factors, with type and stage being the main determinants. Overall, thymomas have better survival outcomes than thymic carcinomas because of their less aggressive nature and lower tendency to spread beyond the original site.
Early-stage thymomas have excellent survival rates, especially when complete resection is possible. Patients with Stage I and II thymomas have 5-year survival rates above 90% when they receive adequate treatment. The survival rate of thymus gland cancer improves when surgery is combined with adjuvant therapy such as radiation.
Advanced-stage thymomas have variable outcomes. Stage III and IV require multimodal treatment, often with neoadjuvant chemotherapy to shrink the tumour before surgery. Even in these challenging cases, 5-year survival rates can be as high as 70-80% with therapy at specialist centres.
Unfortunately, thymic carcinomas have lower survival rates due to their aggressive nature. Thymic carcinoma is more likely to recur than thymoma and requires intense surveillance and often additional treatment. But aggressive treatment combining surgery, chemotherapy and radiation can achieve meaningful survival. Some patients can have long disease-free periods.
Age, overall health, and response to treatment also impact survival. Younger patients tend to tolerate treatment better and often experience more favourable outcomes. Presence of associated conditions like myasthenia gravis can complicate treatment, but doesn’t necessarily worsen long-term prognosis if the condition is appropriately managed.
Long-term follow-up is crucial as thymomas can recur years after treatment completion, and patients are at higher risk of developing other cancers. This requires lifelong surveillance with regular imaging and clinical assessments.

What Causes Death in Thymus Gland Cancer Patients?
Understanding mortality in thymus gland cancer helps patients and families prepare for the coming challenges and also emphasises the importance of comprehensive care. Deaths from thymoma usually occur from several mechanisms often years after initial diagnosis, due to the slow-growing nature of many thymic tumours.
Local disease progression is a major concern, especially when tumours compress vital chest structures. Advanced tumours can compress airways or major blood vessels and cause respiratory failure or cardiovascular complications. Superior vena cava syndrome, whilst treatable, can be life-threatening if compression develops rapidly. That’s why symptoms of SVC syndrome must be handled immediately.
Distant metastases, although less common in thymomas than in thymic carcinomas, can affect vital organs, including the liver, bones and brain. Thymic carcinomas grow faster and are more likely to spread to other parts of the body, such as bones and the liver, and are harder to cure. When multiple organ systems are involved, treatment options may be limited.
It’s also important to acknowledge that treatment-related complications can cause death, especially in patients with significant comorbidities. Major thoracic surgery has inherent risks, especially in older patients or those with compromised lung function. Chemotherapy and radiation therapy can cause long-term effects like secondary cancers, cardiac toxicity, and pulmonary fibrosis.
Associated autoimmune conditions, especially myasthenia gravis, can complicate the clinical course. Myasthenic crises can be life-threatening and require intensive medical management and, in dire situations, mechanical ventilation. Proper management of these conditions requires specialist expertise and coordinated care between multiple specialists.
Recurrent disease poses ongoing challenges as treatment options may become limited with each recurrence. Thymic carcinomas often recur, and management of recurrent disease requires careful balance between aggressive treatment and quality of life considerations.

Advanced Minimally-Invasive Surgical Techniques
Thymus gland cancer treatment has revolutionised with the development of minimally invasive techniques that reduce patient discomfort while maintaining excellent cancer control outcomes. The traditional approach required large chest incisions to remove the masses. Contemporary surgical methods offer patients significant benefits in terms of recovery time, cosmetic results and overall experience.
Video-assisted thoracic surgery (VATS) is a significant advancement in the resection of thymic tumours. This technique uses small incisions (3-4 in total, 1-2 cm in length) through which surgeons insert a thoracoscope, a thin, flexible instrument with a high-definition camera, allowing a detailed visualisation of the chest cavity. Through these ports, surgeons manipulate special instruments to dissect and remove the thymus gland and associated tumour while maintaining excellent visualisation of critical structures like major blood vessels, nerves, and pericardium around the heart.
Robotic-assisted thoracic surgery (RATS) is the latest advancement in minimally invasive techniques for thymus gland cancer. This technology uses sophisticated robotic systems that provide surgeons with greater precision, dexterity and 3D visualisation capabilities that surpass human limitations. During robotic thymectomy, the surgeon controls the robotic arms from a console, translating hand movements into precise instrument movements inside the patient’s chest. The system filters out hand tremors and scales movements, allowing for very delicate dissection around critical structures in this confined space. This is particularly useful when the tumours are close to major blood vessels or the pericardium.
Both VATS and RATS robotic approach offer patients several advantages over traditional open surgery. Recovery times are reduced from weeks to days, allowing many patients to return to normal activities in 1-2 weeks instead of 6-8 weeks after open surgery. Pain levels decrease significantly, often eliminating the need for strong pain medications during recovery.
Patient selection is key for minimally invasive approaches. Very large tumours or those with extensive involvement of surrounding structures may still require open surgical techniques. But the majority of thymus gland cancers are suitable for minimally invasive resection when done by experienced thoracic surgeons.

Living with Thymus Gland Cancer
Surviving thymus gland cancer involves ongoing medical surveillance and attention to quality of life factors that enable patients to get back to meaningful lives. The journey extends beyond initial treatment and requires a long-term partnership between patients and their healthcare teams.
Follow-up care protocols usually involve regular imaging studies and clinical assessments to detect potential recurrences as early as possible. Most centres recommend CT scans every 6 months for 2 years, followed by annual scans thereafter, but individual schedules may vary based on specific risk factors.
Patients with associated autoimmune conditions require additional specialised care. Myasthenia gravis management often requires neurologists who specialise in neuromuscular disorders, medications that improve muscle strength, and ongoing monitoring for potential complications. Many patients find that proper management of myasthenia gravis significantly improves their quality of life and functional capacity, with most achieving excellent functional outcomes within a few months of treatment.

The Way Forward: Find the Right Care
You have time on your side when diagnosed with thymus gland cancer. Unlike some aggressive cancers, most thymic tumours grow slowly, allowing for a thorough evaluation and careful treatment planning. This will enable you to gather multiple opinions and ensure your treatment plan incorporates the latest approaches. Early intervention is better, but even patients with advanced disease can get good results with the proper treatment.
If you or a loved one has been diagnosed with thymus gland cancer, don’t go through this journey alone. The team at Neumark Lung & Chest Surgery Centre combines surgical expertise with compassionate care. Our specialists use the latest minimally invasive surgical techniques, including robotic-assisted and video-assisted thoracic surgeries, to get the best outcomes with shorter recovery times. We recognise that every patient is unique, and we will develop a personalised treatment plan tailored to your specific needs and circumstances. Contact us today to book a consultation and start your journey to expert care and hope.

