Video-assisted thoracoscopic surgery (VATS) is a minimally invasive surgical technique used to diagnose and treat a variety of conditions within the chest or thorax. Unlike traditional open surgery, which involves large incisions and rib spreading, VATS uses small cuts and specialised tools, reducing trauma to the body. A tiny camera called a thoracoscope, transmits live images inside the chest to a video monitor, allowing the surgeon to operate precisely.
This advanced technique is preferred for many thoracic procedures, offering benefits such as decreased pain, faster recovery, and a shorter hospital stay.
Why Is VATS Performed?
Surgeons use VATS to address a wide range of thoracic conditions, including:
- Cancer Diagnosis and Treatment: Tissue biopsies for lung, mesothelioma, and other chest cancers.
- Lung surgeries: Cancer resections in the lung and lung volume reduction surgery.
- Pleural Effusion Management: Removal of excess fluid or air from the space between the lungs and the chest wall.
- Esophageal and Stomach Conditions: Surgeries such as esophagectomy (removal of part, or all, of the oesophagus) and repair of hiatal hernias.
- Hyperhidrosis Treatment: A procedure to relieve excessive sweating.
- Thymectomy: Removal of the thymus gland, often performed for myasthenia gravis or other conditions.
- Heart, Rib and Diaphragm Procedures: Certain minimally invasive heart surgeries and surgeries involving the spine or diaphragm.
What to Expect During VATS
Preparation
Before the procedure, patients undergo various tests to ensure they are suitable candidates for VATS as surgery. These may include imaging tests, lung function tests, blood work and a heart evaluation. Your doctor will also provide detailed instructions to prepare for surgery, such as fasting requirements and medication adjustments. It’s important that you’re mentally prepared for the procedure as well. If required, your doctor can go through greater detail about the exact process.

Procedure
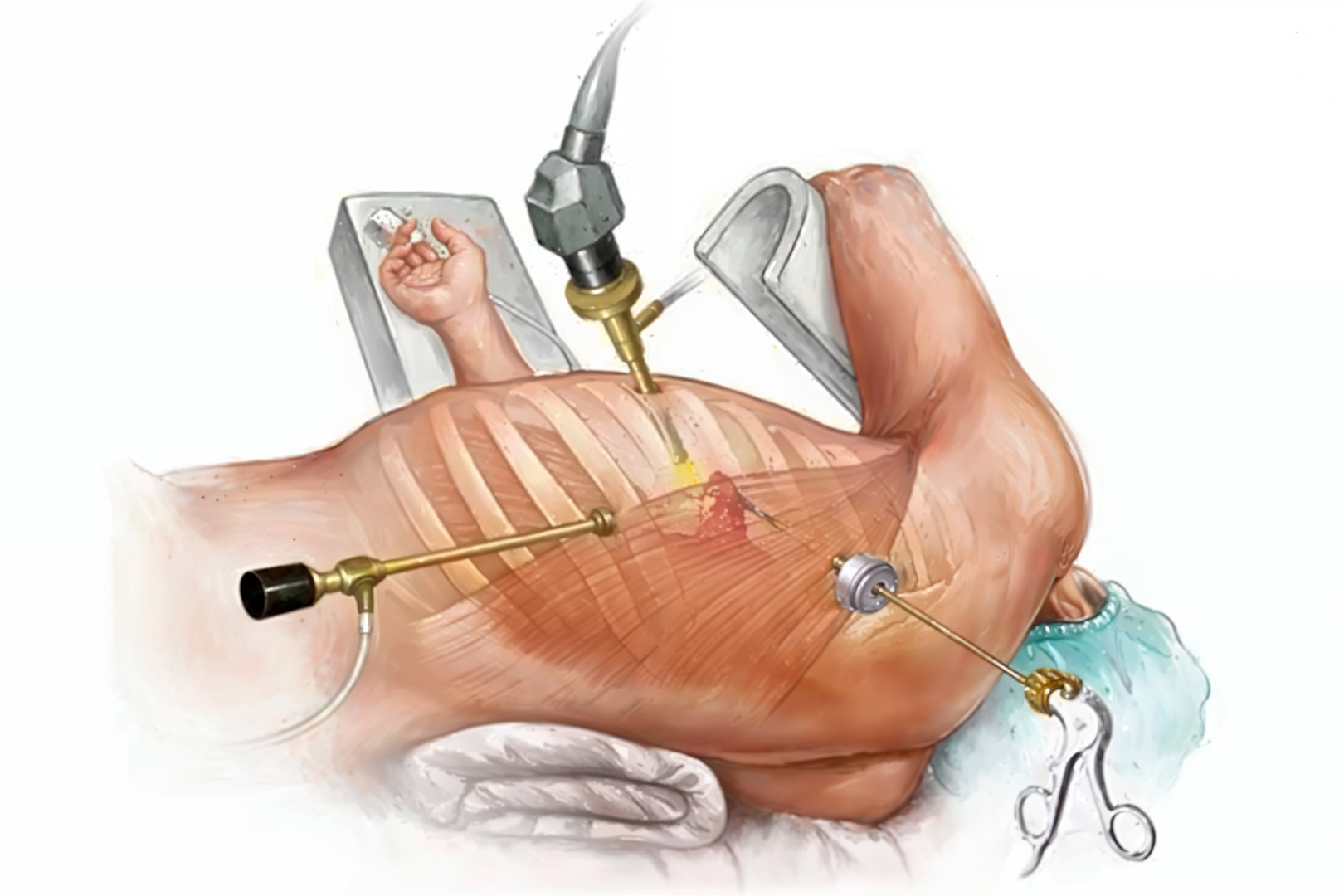
VATS is performed under general anaesthesia, ensuring the patient is in a sleep-like state. The surgeon makes small incisions in the chest wall, through which the thoracoscope and surgical instruments are inserted. Depending on the procedure, or aims of the surgery, the surgeon may:
- Remove tissue for a biopsy
- Excise part of the lung or lymph nodes
- Drain fluid or air from the chest cavity
- Repair structures such as the oesophagus or diaphragm
A chest tube is placed at the end of the surgery to drain any remaining fluid or air and assist lung re-expansion. The procedure typically takes 2 to 3 hours, although this may vary depending on the complexity of the case.
Recovery
Most patients stay in the hospital for a few days following VATS. During this time, medical staff monitor for complications and manage pain. Once discharged, patients are advised to rest and gradually return to daily activities. The full recovery time for VATS may take several weeks, but many individuals experience a quicker return to normalcy than open surgery.
Risks and Complications
While the VATS success rate is high, it carries some risks, such as all surgeries. Potential complications include:
- Pneumonia or other infections
- Bleeding
- Nerve damage
- Air leaks or partial lung collapse
- Blood clots
- Reactions to anaesthesia
However, many of these complications are present in other forms of lung surgery. In many cases, they are more likely to occur when performed using a process not involving VATS.
Benefits of VATS
Video-Assisted Thoracic Surgery (VATS) represents a significant advancement over traditional thoracic surgical approaches, offering patients several compelling benefits. VATS’s smaller incisions translate to notably less postoperative pain, while the minimally invasive nature of the procedure typically results in shorter hospital stays and faster overall recovery times.
Patients also benefit from a reduced risk of infection, as the technique minimises tissue trauma and exposure during surgery. Aesthetically, VATS leaves minimal scarring compared to traditional open surgery, as it requires only small incisions, which can have a serious psychological benefit for many patients.
VATS proves to be an equally effective alternative to conventional surgery for patients who qualify, with the added advantage of enabling a quicker return to daily activities.
Who Is Eligible for VATS?
Determining whether a patient qualifies for Video-Assisted Thoracic Surgery (VATS) involves carefully evaluating multiple factors, including their specific condition, overall health status, and surgical history. Many patients with early-stage lung cancer, pleural effusion, or other localised thoracic conditions make excellent candidates for this minimally invasive approach.
However, VATS may only be suitable for some. Patients with extensive previous chest surgeries or significant scarring might require traditional surgical methods instead, as scar tissue can affect the feasibility. Given these considerations, a thorough consultation with an experienced thoracic surgeon becomes crucial in determining the most appropriate surgical approach for each case.
Uniportal VATS Surgery at Neumark
Through a specialised technique called Uniportal Video-Assisted Thoracic Surgery (U-VATS), skilled surgeons can perform a wide range of thoracic procedures, from biopsies to complex lung resections, through a single small incision. This approach has significant benefits over traditional thoracic surgery, which requires a large chest wall incision and often results in considerable pain, scarring, and lengthy recovery periods.

U-VATS’s combination of minimal invasiveness and enhanced surgical precision makes it particularly revolutionary. By utilising just one small incision between the ribs, surgeons can significantly reduce surgical trauma while maintaining optimal access to the surgical site. The procedure employs a thoracoscope, a sophisticated device with a fibre-optic video camera, that provides Neumark’s surgical team with real-time visualisation of the chest cavity. This enhanced view, coupled with the less invasive approach, enables greater surgical precision and typically leads to better outcomes with fewer complications.
If you’re considering thoracic surgery or have been diagnosed with a condition that might require intervention, consult with Dr Harish Mithiran at Neumark Lung & Chest Surgery Centre for a thorough evaluation to determine if VATS is the right choice for your treatment.

