What to Know About Lung Nodules
Finding a lung nodule on a routine chest X-ray or CT scan can be scary. These small, round or oval lung lesions, called pulmonary nodules, appear as white spots on imaging studies. While the word ‘nodule’ may sound ominous, it should be noted that over 95% of lung nodules are benign in non-smokers.
Lung nodules are very common. Studies indicate that up to 50% of adults who undergo chest CT will have at least one lung nodule. Most are harmless, like old infections, traces of inflammation, or benign tumours. However, a small percentage may be early signs of lung cancer. Understanding when to monitor lung nodules is important for both patients and physicians.
What Is a Lung Nodule?
A lung nodule is a small abnormal growth in the lung tissue, usually less than 10mm in size. Finding a lung nodule can be alarming, but most are benign, meaning they are not cancerous. These benign nodules can result from various causes, such as prior infections, inflammation, or scar tissue.
Some lung nodules can, however, be malignant or cancerous, so it’s important to determine their nature. Infections, autoimmune diseases such as rheumatoid arthritis, and environmental toxins can cause lung nodules. Understanding the underlying cause of the nodule helps to treat and manage it effectively.
Key Factors to Consider
When evaluating whether a lung nodule is concerning, thoracic specialists consider several important factors, such as the nodule’s size, imaging appearance, and the patient’s medical history, including smoking status. These factors help distinguish benign from malignant lung nodules, informing the need for further testing and treatment.
Size Matters
Nodule size is one of the most important predictors of malignancy risk. Generally, nodules less than 6mm (about 1/4 inch) are at a very low risk of being cancerous. These tiny nodules are usually followed up with imaging tests rather than immediate intervention. Nodules 6-10mm fall in the intermediate risk category with about a 1-5% chance of being cancerous, depending on other risk factors. More importantly, nodules larger than 10mm (about 1/2 inch) are concerning, with the risk of malignancy increasing with size. If other risk factors are present, nodules larger than 20mm have a 50% chance of being cancerous.
Growth Pattern and Changes Over Time
Perhaps more important than the nodule’s initial size is its behaviour over time. Cancerous nodules typically double in volume every 100 to 400 days, a growth pattern that may not appear significant at first glance, especially when only considering their diameter.
When evaluating a lung nodule, your thoracic specialist will often recommend follow-up imaging tests at intervals based on its characteristics to see if its size changes. A nodule that has been stable in size for two years is usually benign. Any measurable growth during follow-up periods increases the likelihood of malignancy and warrants more aggressive evaluation.
Appearance and Characteristics of Benign Lung Nodules
The radiographic appearance of lung nodules provides important clues about their nature. Some nodules may arise from prior lung infections, leading to inflammation and granulomas. Features that are a cause for concern include:
- Irregular or spiculated (spiky) margins rather than smooth, well-defined borders
- Solid appearance vs ground-glass opacity
- Upper lobe location, where lung cancers are more common
- Presence of internal cavitation or calcification patterns not typical of benign conditions
These visual characteristics help radiologists and thoracic surgeons determine when to worry about lung nodules and how aggressively to pursue treatment.

Personal Risk Factors
When deciding whether to worry about lung nodules, your personal risk profile plays a significant role. Key factors include:
- Age: Nodules in patients older than 50 are at a higher risk than those in younger individuals.
- Smoking history: Current or former smokers have a much higher risk of malignancy when a nodule is found.
- Family history: A strong family history of lung cancer increases the likelihood of the nodule being malignant.
- Previous malignancy: Patients with previous cancers, especially lung cancer or cancers that metastasise to the lungs, are at higher risk.
- Environmental exposures: Occupational exposure to carcinogens such as asbestos, radon, or uranium increases concerns about nodular malignancy.
These factors will influence how your thoracic surgeon will manage your lung nodule diagnosis.
Detection and Diagnosis
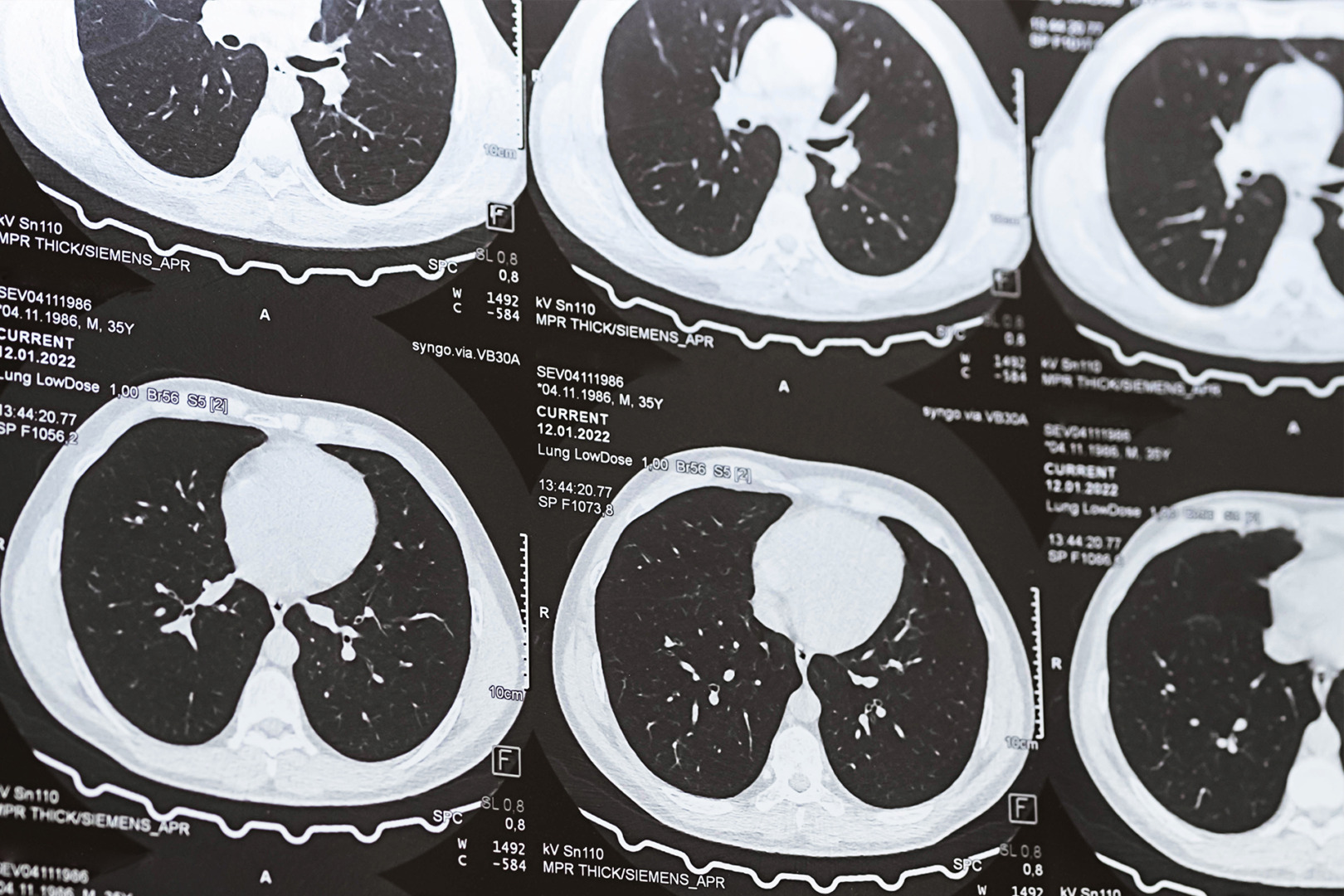
Lung nodules are often detected incidentally during imaging performed for unrelated indications. Common imaging modalities for detecting lung nodules include chest X-rays and computed tomography (CT) scans. CT scans are more valuable as they are more sensitive and can detect smaller nodules that may not be visible on a standard X-ray. CT scans also provide detailed information about the nodule’s size, shape and location within the lung.
If a lung nodule is found, further evaluation is usually recommended to determine if it’s benign or malignant. In some cases, a biopsy is necessary: a small tissue sample is taken from the nodule and examined under a microscope for the presence of cancer cells. Techniques such as CT-guided needle biopsy or endobronchial ultrasound are commonly used to obtain these tissue samples with minimal patient discomfort.

Lung Cancer Screening
Lung cancer screening is a proactive approach to detecting lung cancer early, especially in high-risk individuals. The primary tool for lung cancer screening is a low-dose CT scan of the chest, which can detect lung nodules and other abnormalities that may indicate cancer. This screening is recommended for individuals 55 to 74 with a significant smoking history, with significant smoking defined as at least 1 pack of cigarettes per day for 30 years or more.
The goal of lung cancer screening is early detection, which can improve treatment outcomes for lung nodules and reduce cancer deaths. By detecting lung cancer early, when it’s more treatable, patients have better chances of recovery.
Early Detection Matters
Early detection of lung nodules and lung cancer is key to better treatment outcomes and cancer death reduction. Lung cancer often doesn’t cause symptoms in its early stages, so it can go unnoticed until it has advanced and spread to other parts of the body. That’s why early detection through screening and diagnosis is crucial, as it can catch lung cancer before it spreads.
By detecting lung cancer early, patients have a higher chance of successful treatment and a lower risk of cancer death. When lung cancer is detected early, treatments like surgery, chemotherapy and radiation therapy are more effective. The choice of treatment depends on the stage and type of cancer, but early-stage lung cancer has a better prognosis.
When to Act Fast for Lung Nodules
While many lung nodules can be safely monitored, certain scenarios require prompt evaluation rather than watchful waiting. Consider seeking immediate consultation when:
- A newly found nodule exceeds 8mm in a high-risk individual.
- A previously stable nodule shows growth on follow-up imaging.
- The nodule may present with concerning symptoms such as unexplained weight loss, a persistent cough, or haemoptysis (coughing up blood).
- Multiple nodules appear suddenly without a clear explanation.
In these situations, your thoracic specialist may recommend additional imaging studies, minimally invasive biopsy or, in some cases, surgical removal of the nodule for definitive diagnosis.

Modern Approaches in Lung Cancer Screening
Thoracic medicine has made significant progress in the evaluation of nodules. Today, we have a range of options available to better understand your lung nodules:
- Advanced imaging: High-resolution CT scans, PET scans and other modalities can provide details about the nodule’s characteristics.
- Minimally invasive sampling: Techniques such as CT-guided needle biopsy and endobronchial ultrasound enable tissue sampling with minimal patient discomfort.
- Risk calculator models: Sophisticated algorithms can estimate cancer probability based on nodule features and patient characteristics.
- Genetic and molecular testing: When tissue samples are obtained, advanced molecular testing can identify genetic signatures of malignancy.
These modern approaches have greatly improved our ability to decide when to worry about lung nodules and when to reassure patients that monitoring is sufficient.
Robotic-Assisted Thoracic Surgery (RATS) for Lung Nodules
Robotic Thoracic Surgery (RATS) has revolutionised the approach to lung nodule removal surgery and other thoracic conditions. This advanced technique utilises a robotic system that the surgeon controls from a console. The system translates the surgeon’s hand movements into precise, scaled-down motions of tiny instruments inside the patient’s chest. High-definition 3D cameras provide a magnified, detailed view of the surgical site, offering unprecedented visualisation of the lung tissue and surrounding structures.
The robotic system’s articulated instruments can rotate 360 degrees and bend in ways that exceed human wrist capabilities, enabling intricate manoeuvres in confined spaces. This level of dexterity is particularly beneficial when dealing with nodules in hard-to-reach areas of the lung or when working around delicate structures like blood vessels and nerves.
Robotic thoracic surgery for lung nodules usually involves making 3 to 4 small incisions, each approximately 8mm, through which the camera and instruments are inserted. This minimally invasive approach results in less tissue trauma, reduced postoperative pain, and quicker recovery times compared to traditional open surgery. Patients often experience shorter hospital stays and can return to normal activities sooner.
It is worth noting that the procedure generally takes longer than traditional approaches, which can be a consideration for certain high-risk patients.

Uniportal Video-Assisted Thoracic Surgery for lung nodules
Uniportal Video-Assisted Thoracic Surgery (U-VATS) represents another significant leap in minimally invasive thoracic surgery. This technique involves making a single incision, typically 3-5cm long, usually between the ribs on the side of the chest. The surgeon inserts a video thoracoscope and specially designed instruments to perform the procedure through this single port.
The uniportal approach offers several advantages. The single incision results in less postoperative pain than multi-port VATS or open surgery. It also leads to better cosmetic outcomes, which can be particularly important for some patients’ psychological states. The technique allows for direct visualisation of the target area, and the approach angle closely mimics that of open surgery, making it more intuitive for surgeons trained in traditional techniques.
Uniportal VATS is particularly effective for peripheral lung nodules and straightforward procedures. In experienced hands, it can be used for wedge resections, lobectomies, and even more complex operations. Reduced tissue trauma often leads to faster recovery and shorter hospital stays.
However, the single-incision approach can limit instrument triangulation, thereby making some manoeuvres more complex than those in multi-port techniques. This can be particularly challenging when dealing with centrally located tumours or when an extensive lymph node dissection is required. Your thoracic surgeon will take into account your specific condition and discuss with you which option is most appropriate for your lung nodules.

Contact Neumark’s Lung Nodule Specialists
When to worry about lung nodules depends on a combination of factors, including size, growth pattern, appearance, and your personal risk profile. While most lung nodules are benign, proper evaluation and follow-up are necessary to identify the dangerous minority that are early cancer.
At Neumark Lung & Chest Surgery Centre, we understand the medical and emotional aspects of lung nodule management. Our team uses the latest technology to evaluate nodules accurately while providing the reassurance and guidance patients need during this anxious time.
If you have been diagnosed with a lung nodule or have concerns about your lung health, contact Neumark Lung & Chest Surgery Centre today. Our expert team will comprehensively assess you, guide you through your options, and provide individualised care to treat your lung nodules.

