As a thoracic surgeon with over two decades of experience, I’ve encountered my fair share of medical emergencies. However, few conditions demand as swift and decisive action as tension pneumothorax. This potentially fatal condition occurs when air accumulates in the pleural space between the lung and chest wall, creating a one-way valve effect that progressively collapses the lung and shifts the mediastinum, the space in your chest that holds your heart and pleural cavities. The result? A rapidly deteriorating condition where the very next breath could be the patient’s last.
It’s worth understanding the complexities of tension pneumothorax, including its underlying causes and the latest advancements in treatment. Whether you are a medical professional looking to update your knowledge, or someone interested in learning more about this critical condition, it’s important to know how to manage this thoracic emergency.
Understanding Tension Pneumothorax
To truly grasp the gravity of tension pneumothorax, we must first understand the delicate balance within our chest cavity. In normal circumstances, the lungs expand and contract within a closed system, facilitated by negative pressure in the pleural space. When this system is compromised, a life-threatening emergency ensues.
Tension pneumothorax occurs when air enters the pleural space but cannot escape, creating a pressurised environment. This environment then progressively collapses the affected lung and pushes the heart and major blood vessels toward the opposite side. Needless to say, this is incredibly bad for your body and health. This shift can dramatically reduce cardiac output and venous return (the rate of blood flow back to your heart), leading to cardiovascular collapse if left untreated.
Tension Pneumothorax Causes
The causes of tension pneumothorax are varied, but they all share a common thread: a breach in the integrity of the lung or chest wall. Some of the most common causes include:
- Trauma: Penetrating or blunt chest injuries can create an entry point for air.
- Iatrogenic: Medical procedures like central line placement or mechanical ventilation can inadvertently introduce air.
- Underlying lung disease: Conditions such as COPD or cystic fibrosis can increase the risk of spontaneous pneumothorax, which may progress to tension pneumothorax.
- Barotrauma: Rapid changes in ambient pressure, such as during scuba diving or air travel, can cause alveolar rupture.
It’s important to note the distinction between pneumothorax vs tension pneumothorax. While a simple pneumothorax involves air in the pleural space, it lacks the progressive pressure buildup characteristic of tension pneumothorax. This difference is vital in both diagnosis and management.
It’s also worth noting the differences between tension vs spontaneous pneumothorax. Spontaneous pneumothorax simply describes the method in which pneumothorax develops, i.e. spontaneously. Tension pneumothorax is a type of pneumothorax that can develop from a case of spontaneous pneumothorax, or it can be an acquired pneumothorax, meaning an external incident like an injury or trauma causes it.
Recognising Tension Pneumothorax Signs and Symptoms
The signs and symptoms of tension pneumothorax can escalate quickly, often within minutes, making swift recognition crucial. As a thoracic surgeon, I’ve seen firsthand how identifying these urgent signals can be life-saving. The key indicators to watch for tension pneumothorax treatment include:
- A sudden, intense chest pain that feels like a sharp stabbing sensation, often accompanied by a rapid and frightening onset of shortness of breath, as if every breath is a struggle for air.
- Tachycardia and hypotension, where the heart races in a desperate attempt to pump enough blood, but blood pressure drops dangerously low, leaving the body in a state of shock.
- Distended neck veins are visibly swollen as blood backs up in the veins due to the increased pressure in the chest cavity.
- Tracheal deviation away from the affected side, is a critical sign where the windpipe is visibly pushed to the side due to the pressure building up in the chest.
- Absent breath sounds on the affected side, where the once rhythmic breath sounds disappear, replaced by a worrying silence that signals a lack of air movement in the lungs.
- Hyper-resonance to percussion on the affected side, where tapping the chest produces a hollow, drum-like sound, indicating trapped air under pressure in the chest cavity.
Any one of these symptoms already sounds frightening enough. But it’s important to note that they’re not just problems in themselves; they are warning signs. It’s essential to recognise them quickly and accurately for timely intervention, which can significantly improve patient outcomes. In mechanically ventilated patients, tension pneumothorax may manifest as sudden cardiovascular collapse, increased airway pressures, and difficulty ventilating.

It’s important to note that tension pneumothorax symptoms can sometimes be subtle, especially in the early stages. This underscores the importance of maintaining a high index of suspicion, particularly in high-risk patients or following certain medical procedures. That’s why it’s not just about tackling tension pneumothorax as it arises; it’s also about management.
Tension Pneumothorax Management
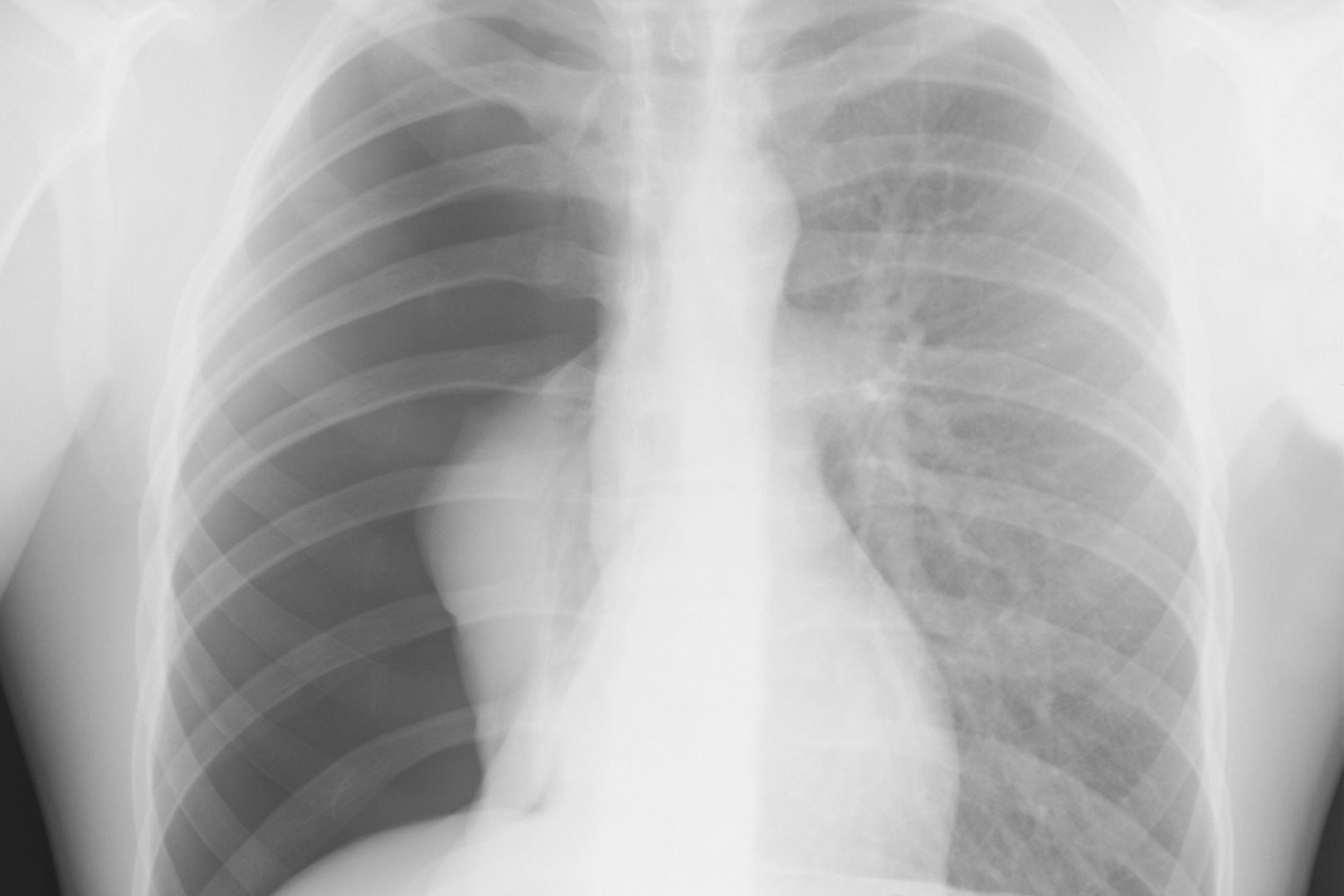
When it comes to tension pneumothorax, time is of the essence. The steps are clear: rapid diagnosis followed by immediate decompression. In most cases, tension pneumothorax is a clinical diagnosis based on the patient’s history, physical examination, and rapid deterioration. While chest X-rays can be helpful, waiting for imaging should never delay treatment in a clinically apparent case.
The first-line treatment is needle decompression, which involves inserting a large-bore needle into the second intercostal space at the midclavicular line on the affected side. The sudden rush of air confirms the diagnosis and provides immediate, albeit temporary, relief. Following needle decompression, a chest tube (also known as a chest drain) is inserted to provide definitive management. This tension pneumothorax chest drain allows for continuous drainage of air and any accumulated fluid, giving the lung a chance to re-expand.
Throughout the treatment process, supportive care is crucial. This includes oxygen therapy, pain management, and close monitoring. In severe cases, mechanical ventilation may be necessary to support oxygenation and ventilation. This comprehensive approach ensures the best possible outcome.

While the fundamental principles of tension pneumothorax management remain unchanged, advancements in thoracic surgery have opened up new avenues for treatment, particularly in complex or recurrent cases.
Uniportal Video-Assisted Thoracoscopic Surgery (U-VATS)
As a thoracic surgeon at the forefront of minimally invasive techniques, I’ve witnessed firsthand the transformative impact of Uniportal Video-Assisted Thoracoscopic Surgery (U-VATS).
U-VATS allows us to perform complex thoracic procedures through a single small incision, typically about 3-4 cm in length. This technique offers several advantages over traditional open surgery, including reduced postoperative pain and faster recovery, improved cosmetic results, enhanced visualisation of the thoracic cavity, and the ability to perform diagnostic and therapeutic procedures simultaneously.
U-VATS can be particularly useful in addressing underlying causes or managing complications of tension pneumothorax. For instance, we can use U-VATS to identify and repair air leaks, perform pleurodesis to prevent recurrence, remove blebs or bullae that may have caused the initial pneumothorax, and manage empyema or other infectious complications.

The precision and minimally invasive nature of U-VATS make it an invaluable tool in our arsenal. It allows us to provide definitive treatment while minimising trauma to the patient. This advanced technique has significantly improved our ability to treat complex cases of tension pneumothorax and its associated complications, offering patients better outcomes and quicker returns to their normal lives.
Tension Pneumothorax Complications
While prompt recognition and treatment of tension pneumothorax can be lifesaving, it is crucial to remain vigilant for potential complications. These can include re-expansion pulmonary edema, where rapid re-expansion of a collapsed lung can lead to pulmonary edema in the affected lung.
Another concern is infection, with empyema or pneumonia potentially developing as a result of the initial pneumothorax or its treatment. Some patients may experience chronic pain, manifesting as persistent chest wall discomfort following a tension pneumothorax event.
Without addressing underlying risk factors, recurrent pneumothorax’s always risky.
As thoracic surgeons, our role extends beyond the initial emergency management. We work closely with patients at Neumark Lung & Chest Surgery Centre to address these potential complications and develop long-term management strategies to prevent recurrence. This comprehensive approach ensures that patients receive continuous care and support, minimising the risk of future episodes and improving their overall quality of life.
A Breath of Fresh Air
Tension pneumothorax remains one of the most time-sensitive emergencies in thoracic medicine. Its successful management requires swift action, clinical insight and advanced surgical techniques.
As we refine our understanding of this condition and develop new treatment modalities, the prognosis for patients with tension pneumothorax continues to improve. From rapid needle decompression in the emergency room to advanced U-VATS procedures in the operating theatre, each step in the management pathway plays a crucial role in saving lives.
For medical professionals, maintaining a high index of suspicion and staying updated on the latest management guidelines is paramount. Awareness of the signs and symptoms can lead to earlier presentation and potentially life-saving interventions for patients and the general public.

