Non-small cell lung cancer may sound like a confusing term. In fact, the definition of non-small cell lung cancer, which accounts for about 85% of lung cancer cases, is that it is an umbrella term for several types of lung cancer, including adenocarcinoma, squamous cell carcinoma and large cell carcinoma.
On average, 23 out of 100 people with lung cancer live for 5 years or more after diagnosis. However, this depends a lot on how early the cancer is found, as the life expectancy of Stage 4 non-small cell lung cancer is very different from that of Stage 1. The 5-year survival rate for localised-stage NSCLC is approximately 65%.
Finding lung cancer early is key because the window for life-saving surgery is too late once it metastasises, as evident through non-small cell lung cancer statistics. If caught early and stays localised in the lung, 61 out of 100 people can live for 5 years or more. If the cancer has spread to nearby areas, the number drops to 34. If the cancer has metastasised to other parts of the body, only 7 out of 100 people might live for 5 years or more.
Early-stage NSCLC often presents without symptoms, underscoring the importance of early detection for improved outcomes. Lung cancer screening, such as low-dose CT scans, is recommended to improve early detection rates and prolong the life expectancy of patients with non-small cell lung cancer.

What Does Non-Small Cell Lung Cancer Mean?
Non-small cell lung cancer is the most common type of lung cancer. But how does it grow in the body?
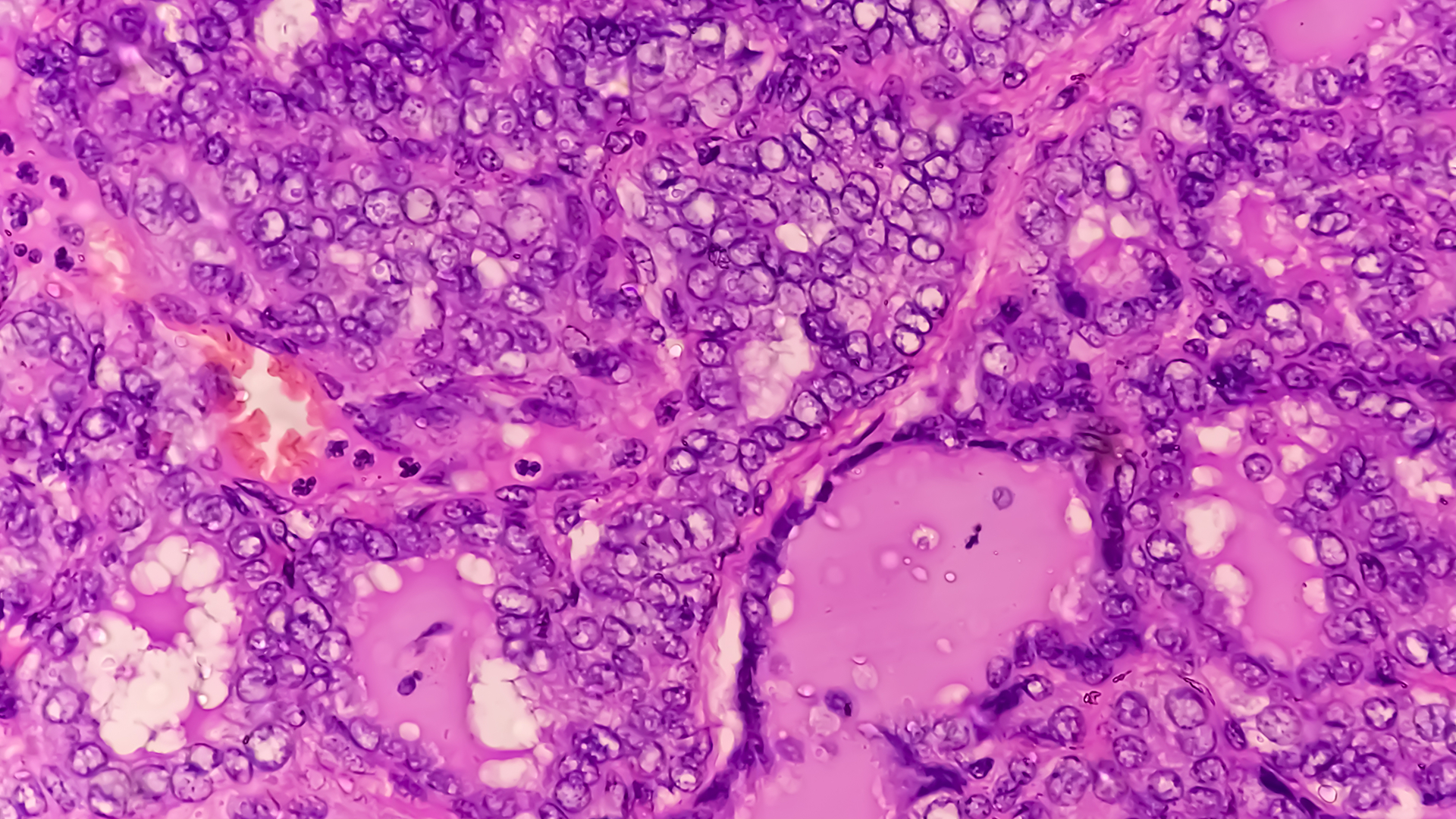
Imagine tiny rebels in your lungs, normal cells gone rogue, reproducing out of control. These cells grow uncontrollably to form tumours called carcinomas, which ravage the lining of your bronchi, bronchioles, and alveoli.
Unlike its small-cell carcinoma cousin, NSCLC grows across the lung surface. This rapid cell division disrupts lung structure and impairs oxygen and carbon dioxide exchange. This leads to shortness of breath, coughing and chest pain, all common non-small cell lung cancer symptoms.
The process of non-small cell lung cancer diagnosis is critical as accurate diagnosis guides treatment and patient outcomes. The disease is influenced by a mix of genetic, environmental and lifestyle factors, with smoking being a significant risk. Other non-small cell lung cancer causes include:
- Secondhand smoke, environmental pollutants, and health conditions such as COPD complicate the picture.
- The patient’s age, overall health and response to treatment also play a role in disease development and prognosis.
- Genetic predisposition, including EGFR mutations, and lifestyle choices underscore the importance of broad prevention strategies.
Early detection of lung cancer and healthy living to reduce risk factors for NSCLC. The staging of non-small cell lung cancer is determined by the TNM classification system, which includes three components: the size of the primary tumour (T), the involvement of lymph nodes (N) and the presence of metastasis (M).

Types of Non-Small Cell Lung Cancer
The prevalence of non-small cell lung cancer is very high, accounting for about 85% of all lung cancer cases. NSCLC is not a single disease but rather a group of related cancers that differ in their behaviour and responses to treatment.
NSCLC is classified into three main types based on the affected cells:
- Adenocarcinoma starts in the mucus-producing cells. The most common type of non-small cell lung cancer is adenocarcinoma in never smokers, accounting for about 40% of lung cancers. It typically starts in the outer regions of the lungs and arises from mucus-producing cells in the small airways. Its slower growth rate than other lung cancers often leads to better outcomes. Adenocarcinoma accounts for about 87.3% of NSCLC in Singapore, which affects both smokers and non-smokers.
- Squamous cell carcinoma originates in the flat cells lining the airways. Squamous cell carcinoma originates in the flat cells lining the bronchi and is more likely to spread to other parts of the body, thus making it more challenging to treat as a form of metastatic non-small cell lung cancer (NSCLC). Squamous-cell carcinoma of the lung is more common in men than in women and is closely related to a history of tobacco smoking.
- Large cell carcinoma is characterised by rapid growth and can occur in any lung region. Large cell carcinoma, a less common type of NSCLC, can happen in any lung area and is aggressive. Large-cell lung carcinoma (LCLC) accounts for approximately 10% of all NSCLC cases; it is a diagnosis of exclusion.
Besides these, there are other rare types of non-small cell lung cancer, such as adenosquamous carcinoma and sarcomatoid carcinoma. These subtypes combine features of different cell types or have unique characteristics and may require special treatment approaches.
Non-Small Cell Lung Cancer in Non-Smokers
Lung cancer is not exclusive to smokers anymore. Still, Dr Harish Mithiran, senior consulting thoracic surgeon at Gleneagles and Mt Alvernia hospitals in Singapore, stresses the undeniable link between tobacco use, lung health, and lung carcinoma. Exposure to environmental pollutants and carcinogens also contributes to the incidence of non-small cell lung cancer in Singapore. Family history of lung cancer also contributes to increased risk and is considered along with other risk factors such as genetic predispositions and environmental exposures.
“Unfortunately, the disease often goes undetected until it has spread to other parts of the body. This is more often the case than early detection”, Dr Mithiran says. “With non-smokers getting this fatal disease, getting screened early is the best prevention against silent progression to advanced stages.”
Luckily, there are many non-small cell lung cancer treatments, so there is hope for those diagnosed.
With the advancement of clinical understanding and depending on the lung cancer stage and characteristics of the disease, surgical interventions, chemotherapy, radiation therapy and even targeted genetic therapies can be ways for management of non-small cell lung cancer, and potentially cure non-small cell lung cancer.

Symptoms You Should Never Ignore
Non-small cell lung cancer signs and symptoms are similar to those of less serious conditions or develop due to long-term smoking. This is why delayed diagnoses occur in about 80.7% of males and 76.8% of females.
Early detection is key. The 5-year survival rate for Stage 4 NSCLC in Singapore is between 5% to 9%. However, survival rates vary widely depending on the cancer characteristics, treatments and the patient’s overall health.
The most common red flag is a persistent cough that does not go away or changes significantly. Other key lung cancer symptoms include:
- Coughing up blood (haemoptysis): This is a warning sign that requires immediate medical review.
- Chest pain: Especially pain that is constant, dull or worsens with deep breathing or coughing.
- Shortness of breath (dyspnoea): Feeling breathless after light activity or even at rest.
- Persistent respiratory infections: Recurring bronchitis or pneumonia that does not resolve with antibiotics.
- Unexplained weight loss and fatigue: Systemic symptoms seen when cancer has progressed.
When evaluating patients with these symptoms, a complete blood count is often performed as part of the initial assessment to detect hematologic abnormalities or signs of metastasis.
For those aged 55-80 with a significant smoking history, annual screenings offer the best chance for early detection of lung cancer and improving survival rates. Low-dose CT scans are a window into your lungs, allowing our lung specialists to spot abnormalities before symptoms occur. This early detection can be the difference between living a healthy life and a more brutal fight against cancer.

Non-Small Cell Lung Cancer Diagnosis in Singapore
When cancer is suspected, further tests like biopsies and genetic testing are necessary for developing personalised treatment for NSCLC.
A diagnosis at Neumark begins with a thorough clinical assessment, including review of your medical history, evaluation of your exposure to NSCLC risk factors, and physical examination. Pharmacologic therapy for smoking cessation may be recommended as part of comprehensive risk reduction. This is followed by imaging.
A chest X-ray may detect an abnormality, but a CT scan provides detailed cross-sectional images that are essential for determining the tumour’s size and location. A PET scan (Positron Emission Tomography) is often used to see if the cancer has spread to other parts of the body, a process known as staging. Detection of metastatic disease, where cancer has spread beyond the primary lung site to distant organs, is critical for prognosis and treatment options.
Confirmation of non-small cell lung cancer requires a tissue sample. Lung biopsies, whether performed by bronchoscopy to visualise and collect tissue or by needle or incision biopsy to remove lung tissue, are necessary for analysis. After a confirmed NSCLC diagnosis, genetic testing analyses your cancer’s specific traits, looking for molecular markers (such as EGFR, ALK, or PD-L1 mutations), so that a tailored treatment plan can be developed.
For patients with specific genetic mutations, participation in a clinical trial may be considered to access novel targeted therapies or immunotherapies. Common mutations that can be targeted in NSCLC include EGFR, ALK, RAS, BRAF and ROS1.
Neumark streamlines this process for patients in Singapore, coordinating all necessary investigations at our partner hospitals, Gleneagles Hospital on Napier Road and Mount Alvernia Hospital on Thomson Road.

Non-Small Cell Lung Cancer Treatment
The approach to NSCLC is based on a few key factors: the extent of the cancer’s spread (the stage), your general health and age and the presence of specific genetic and protein markers that may affect treatment. For non-small cell lung cancer caught in the early stages before it has spread, patients can have minimally invasive surgery options that aim for the best outcomes.
Surgical resection is the main treatment option for early-stage disease, with wedge resection considered a less invasive option for select patients who may not tolerate a lobectomy.
When cancer has spread beyond the lungs, the approach to treatment for NSCLC goes beyond surgery. Your lung cancer surgical team, consisting of multidisciplinary specialists from various fields (surgical oncology, medical oncology and radiation oncology), will decide on the best treatment option or combination of treatments for you after a thorough assessment.
Treatments for lung cancer of non-small cell type may include:
- Chemotherapy: To eliminate cancer cells throughout the body, often used before surgery (neoadjuvant chemotherapy) to shrink a tumour, or after surgery (adjuvant chemotherapy) to kill remaining cancer cells, or as primary treatment for advanced disease. Chemotherapy combined with radiation therapy is a standard approach for certain stages, such as stage IIIB, while sequential chemotherapy may be considered as an alternative strategy.
- Radiation Therapy: Focused beams to target and kill cancer cells, often used alone or combined with chemotherapy. Advanced radiation treatment options, such as stereotactic body radiation therapy and continuous hyperfractionated accelerated radiotherapy, offer potential survival benefit in specific cases.
- Targeted Drug Therapy: Targets specific molecular alterations in cancer cells (identified through genetic testing) and provides a customised treatment plan for NSCLC, with fewer side effects than traditional chemotherapy.
- Immunotherapy: Uses drugs to help a patient’s own immune system recognise and attack cancer cells. Adding targeted therapies for specific mutations can significantly improve overall survival in patients with NSCLC compared with standard chemotherapy alone.
For Stage II NSCLC, surgery followed by adjuvant chemotherapy and, if indicated, adjuvant immunotherapy is recommended, with studies showing a survival benefit. For Stage IV NSCLC, where the disease is metastatic, the prognosis is poor, and treatment options are focused on systemic therapy, targeted agents, and palliative treatment to improve quality of life.
EGFR Mutations and Targeted Therapy
Some cases of non-small cell lung cancer are driven by specific genetic changes, such as mutations in the epidermal growth factor receptor (EGFR) gene. These EGFR mutations cause cancer cells to grow and divide uncontrollably, reducing their responsiveness to conventional therapies such as chemotherapy and radiation therapy. Advances in targeted therapy have changed the outlook for patients with these mutations.
By interfering with this pathway, these medications can slow or stop tumour cell growth.
Clinical trials have shown that EGFR inhibitors can significantly improve progression-free survival and overall survival in patients with NSCLC harbouring EGFR mutations, compared to standard chemotherapy. As a result, testing for EGFR mutations is now part of the diagnostic process for NSCLC so that patients can receive the most effective, personalised treatment of non-small cell lung cancer (NSCLC).

Minimally Invasive Thoracic Surgery
Neumark offers minimally invasive surgery options for early-stage non-small cell lung cancer. The goal of surgery is curative: to remove the tumour and any affected lymph nodes (a procedure called a lobectomy or segmentectomy, depending on how much lung tissue is removed) with minimal disruption. For select patients with small peripheral tumours or poor pulmonary reserve, a wedge resection, a less invasive surgical resection technique, may be considered.
Video-Assisted Thoracoscopic Surgery (VATS)
VATS is a standard minimally invasive approach. It involves small incisions (usually 2-3) and a high-definition camera inserted between the ribs to see inside the chest cavity. This allows surgeons to operate with precision and patients to recover more quickly than with open surgery.
- Eligibility: Early-stage NSCLC.
- Benefits: Smaller scars, less pain, shorter hospital stay, faster return to normal activities.
- Limitations & Risks: Not suitable for very large, central or complex tumours. Risks are lower than open surgery but include air leak, bleeding and infection.
Robotic-Assisted Thoracic Surgery (RATS)
RATS uses robotic arms controlled by the surgeon from a console to make tiny incisions. Robotic surgery offers surgeons greater precision, high-magnification 3D vision, and greater dexterity than VATS, potentially better patient outcomes, and the ability to perform complex procedures minimally invasively.
- Eligibility: Most patients who qualify for VATS and sometimes more complex cases.
- Benefits: Enhanced surgical precision and surgeon control; recovery outcomes comparable to VATS (less pain, faster recovery).
- Limitations & Risks: Requires special equipment and training. Risks are similar to VATS.
Uniportal VATS (U-VATS)
U-VATS is the latest in minimally invasive surgery options, performing the entire operation through a single small incision. Dr Mithiran at Neumark is experienced in this technique.
- Eligibility: Selected early-stage tumours.
- Benefits: Further reduction in postoperative pain and faster recovery than traditional VATS, with potentially better preservation of chest wall integrity.
The choice among VATS, RATS, and U-VATS will depend on tumour characteristics and the patient’s overall health. Minimally invasive approaches are core to Neumark’s practice, reflecting our commitment to rapid recovery and better quality of life for our patients.

Metastatic NSCLC Treatment
Metastatic NSCLC refers to non-small cell lung cancer that has spread beyond the lungs to other parts of the body, such as lymph nodes, bones, liver or brain. When NSCLC becomes metastatic, the focus of treatment shifts from cure to disease control, symptom relief, and quality-of-life improvement.
Systemic therapies, including chemotherapy and targeted therapy, are the mainstay of treatment for metastatic NSCLC. In some cases, radiation therapy may be used to relieve symptoms or treat specific areas of spread, such as painful bone metastases or brain lesions. The presence of EGFR mutations or other genetic alterations can inform targeted therapy selection and provide additional options for patients with these mutations.
The prognosis for metastatic NSCLC depends on several factors, including the number and location of metastases, the patient’s overall health, and the presence of specific genetic mutations. While metastatic NSCLC is an advanced cancer, new treatments are improving progression-free survival, and many patients can maintain a good quality of life for extended periods.

Managing Side Effects of Treatment
Treatment for non-small cell lung cancer can bring many side effects, including fatigue, nausea, vomiting, hair loss and changes in appetite. Managing these side effects is an important part of cancer care as it helps patients maintain their strength and well-being throughout their treatment.
Supportive care plays a key role in managing these challenges. This may include medications to control nausea, strategies to manage fatigue, such as regular light exercise and adequate rest, and dietary adjustments to support nutrition. For those experiencing hair loss, options such as wigs, hats, or scarves can help maintain confidence and comfort. Open communication with the cancer care team ensures that side effects are addressed promptly, so that patients can focus on recovery and quality of life.
Recovery and Long-Term Surveillance
The recovery after minimally invasive surgery, like VATS or RATS, is faster than open surgery, but still requires patience. Most patients are discharged from the hospital within 4-7 days. Pain management is prioritised in the first week. We encourage light activity and walking soon after surgery to support lung function. Full recovery and return to normal activities typically take 4-8 weeks, depending on the individual.
After NSCLC treatment, follow-up surveillance is crucial. This involves regular check-ups, blood tests and imaging (usually CT scans) for many years to monitor for any signs of lung cancer recurrence. This long-term monitoring is managed seamlessly through Neumark.
Why Choose Neumark Lung & Chest Surgery Centre
At Neumark Lung & Chest Surgery Centre, patients can access the latest surgical techniques that open up new possibilities for those with lung cancer. Under the leadership of Dr Mithiran, our Lung Cancer Treatment Centre is at the forefront of developing lung cancer treatments and conducting clinical research. This is a patient-centred approach. “We work closely with our patients, involving them in their treatment plans. This partnership is key to their successful journey”, says Dr Mithiran.
In partnership with leading hospitals such as Gleneagles and Mt Alvernia in Singapore, this initiative introduces Neumark’s patients to the latest medical advances. Together, these institutions are leading the way in lung cancer care, offering new hope and better treatment for those with NSCLC. We focus on providing the highest-quality, most precise surgical care with the shortest possible recovery time.
If your doctor has found abnormal lung nodules or if you’re experiencing lung cancer symptoms beyond a cough and suspect something more serious, contact Neumark today for a consultation that could save your life. We will guide you through a comprehensive diagnostic process and offer minimally invasive surgical options at our private practice locations at Gleneagles and Mount Alvernia hospitals in Singapore.

